In its first guideline on pneumonia, NICE recommends that using the test in cases which are unclear could help limit the unnecessary use of antibiotics.
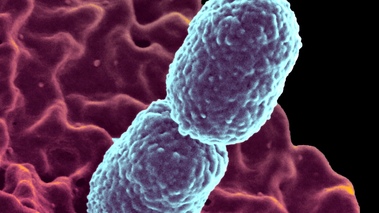
Pneumonia is a swelling of the tissue in the lungs often caused by a bacterial or viral infection of the lungs. The condition affects up to 480,000 adults in the UK each year, and common symptoms include coughing fever or difficulty breathing.
In primary care, the majority of patients without pneumonia present with symptoms of chest infection. This can cause problems with diagnosis, as in the absence of a chest X-ray, it is difficult to determine whether the symptoms are caused by pneumonia or a lower respiratory tract infection which will clear up on its own.
While antibiotics will help those whose symptoms have been caused by a bacterial infection, they will have no effect on those caused by viral infection, and can in fact cause some harm.
NICE recommends that GPs should consider carrying out C-reactive protein test for people presenting in primary care with symptoms of lower respiratory tract infection.
The test should be carried if after clinical assessment a diagnosis of pneumonia has not been made, and it is not clear whether antibiotics should be prescribed.
The guideline outlines the method in which the results of the C-reactive protein test should be used to guide antibiotic prescribing in people without a clinical diagnosis of pneumonia.
Assessing patient risk
Pneumonia can progress rapidly, with around a tenth of those admitted to hospital with the condition ending up in intensive care, where they have a 30 per cent risk of dying.
Consequently, the guideline recommends using a CRB65 score to determine the level of risk of a patient.
The score stratifies patients for risk of death from low to high, and calls for GPs to use clinical judgement in conjunction with the CRB65 score to inform decisions about whether patients need hospital treatment.
Elsewhere, the guideline features recommendations on discharge from hospital information that should be given to patients, and on hospital-acquired pneumonia.
Dr Michael Moore, a GP and member of the Guideline Development Group, explained: “Chest infections provide a tricky problem for GPs, most get better on their own and antibiotics don’t help much at all but some patients have more serious infections and pneumonia. So patients with chesty coughs require careful assessment and thoughtful treatment.
“Without the use of a chest X-ray, pneumonia can be difficult to distinguish from other common respiratory infections. This poses a challenge for GPs working in primary care as chest X-rays are not usually readily available in surgeries or there can be a delay in getting results.
“There is evidence that using a simple blood test, as well as checking signs and symptoms, can help the GP work out what’s happening – so they can help their patient faster.
“The CRP test can be carried out in the GP surgery and it helps decide whether or not treatment with antibiotics is needed. With growing concern over antibiotic resistance, the CRP test is an important tool that can help GPs reduce antibiotic prescribing whilst still being confident about offering patients the best treatment.”
Listen to Dr Michael Moore talk more about the impact of the guideline on primary care practice.
Read transcript Download podcast MP3 5.9 MB
Professor Mark Baker, NICE’s Director of Clinical Practice, said: “Pneumonia is very common. If it is not treated properly, people spend more time in hospital or in the worst cases, it can kill.
“Assessing severity of symptoms is really important to find out the most appropriate way to treat each individual patient. Antibiotics should be offered as soon as possible to people who need them. The recommendations in this new guideline set out how to identify those people with severe symptoms. There will also be people with less severe symptoms who may not need antibiotics at all or who could have a shorter course.
“Accurate assessment of respiratory infections like pneumonia allows healthcare professionals to prescribe treatments responsibly. This both reduces costs and any potential harm from over-exposure to antibiotics. We need to make sure that clinicians are absolutely clear on the best way to treat people with pneumonia, whether that’s in hospital or in the community and this guideline provides that.”