Improving recognition and understanding of frailty on a surgical ward can help to achieve a shorter length of stay and positive outcomes for surgical patients. Furthermore, being in bed or wearing night clothes when not clinically necessary has a negative effect on patients by reinforcing the ‘sick role’ that, although enabled out of compassion and kindness, can lead to unintentional harm.
Simple ideas such as ‘Get up for breakfast’ and ‘Get up and Dressed’ became themes of the month, promoting the appropriate amount of activity and independence for patients and improving multidisciplinary working. Static cycles were installed to reduce the risk of muscle wastage and patients are given pedometers to encourage them to walk.
Guidance for preventing falls in older people, (NICE CG161, 2013), recommends strength and balance training as being beneficial. Likewise, reablement guidance, (NICE NG74, 2017), recommends focusing on developing goals in a collaborative way to optimise independence and wellbeing as well as supporting positive risk taking.
Example
Aims and objectives
NICE guidelines recommend that older people should be assessed for their ability to benefit from interventions to improve strength and balance to prevent falls, using a multifactorial assessment. Individualised muscle-strengthening and balance programmes should be offered, in particular, interventions with an exercise component, (NICE CG161, 2013).
The NICE guideline for intermediate care including reablement recommends developing goals in a collaborative way to optimise independence and wellbeing. This should be achieved by working in partnership with the patient focusing on their motivations and strengths, allowing them to gain confidence in tasks such as dressing themselves and supporting positive risk taking, (NICE NG74, 2017).
The aim of the reablement project is to work with patients, families and staff to improve awareness of exercise, activity and prevention of deconditioning. This includes providing information about dementia care, recognising nutrition and hydration needs, as well as carer’s rights. In addition, through multidisciplinary team working, improving both the recognition and understanding of frailty.
The overall objective of the project is to decrease deterioration of patients by reducing the length of stay in hospital and increase function for patients through the development of personalised daily goals, enabling them to return to their usual place of residence with confidence and independence.
Reasons for implementing your project
Lavenham Ward is a busy 40 bedded emergency surgical ward which includes a surgical admissions unit. Therefore, we have a high turnover of patients with an average of 15 admissions a day to the unit, plus ward attenders, and our care has rightly focused on managing our seriously ill patients effectively whilst maintaining patient flow.
The project was implemented because we would often find that once a frail patient became medically fit for discharge, the long struggle to regain their functional ability to allow them to go home began. Therefore, it was quite apparent due to our nursing care, albeit it through compassion and kindness, their function had significantly reduced and their discharge was delayed whilst we waited for them to be rehabilitated. Sometimes our frail patients never returned home, as they struggled to regain their previous function.
“For every 10 days of bed-rest in hospital, the equivalent of 10 years of muscle ageing occurs in people over 80-years old, and reconditioning takes twice as long as this de-conditioning. One week of bedrest equates to 10% loss in strength, and for an older person who is at threshold strength for climbing the stairs at home, getting out of bed or even standing up from the toilet, a 10% loss of strength may make the difference between dependence and independence.” Professor Brian Dolan
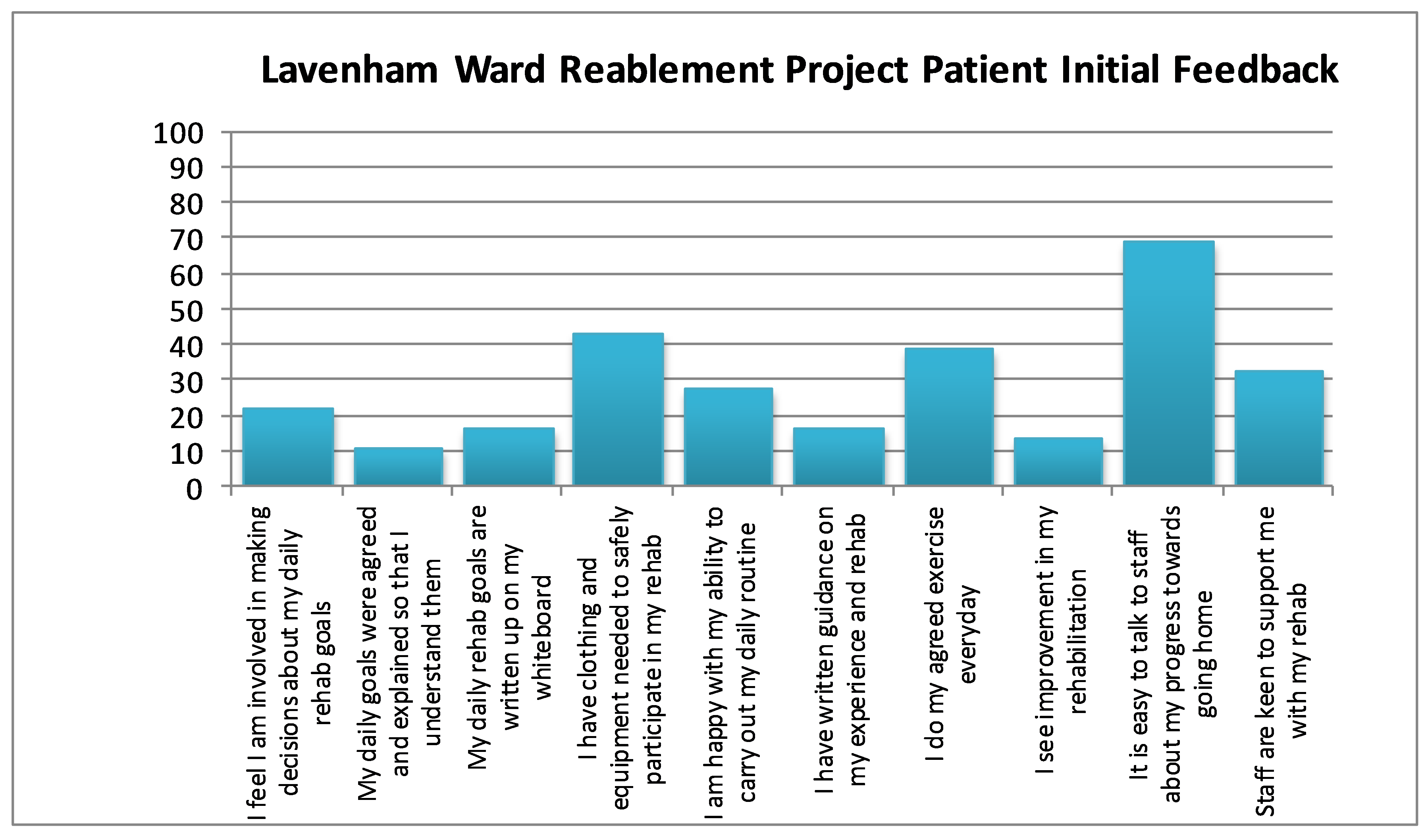
The average length of stay for older patients on Lavenham Ward is 8.4 days, with the longest length of stay over the last three years being 98 Days. With the help of our Ipswich Hospital User Group representative we developed a short patient survey and were surprised to discover that 80% of patients did not know what their daily goals were that would help them to get home, and that 87% didn’t have any written guidance about the exercises they should be doing to achieve their functional goals, (Figure 1).
We recognised that patient flow on the ward could be significantly improved by implementing simple ideas such as ‘Get up for breakfast’ and ‘Get up and Dressed’, enabling a reduction in the length of stay and an increase in more timely admissions. By encouraging independence and allowing patients to take an active role in their health journey this would also increase their mental wellbeing.
Figure 1: Results of a short patient survey before the project was implemented
How did you implement the project
Initial coaching and support for the frailty care project was provided by Eastern AHSN. NICE guidelines recommend a multifactorial assessment for older people at risk of falls, (NICE CG161, 2013). A ‘frailty bundle’ pathway was implemented upon patient admission, with assessment made using the Rockwood frailty score. Measures are put in place for those scoring 4 or above, such as a Food Record Chart, Stool Chart and Input-Output Chart. In addition, the appropriate teams and clinicians are informed, for example, the frailty nurse consultant, dietitians, geriatricians, therapists and specialists such as Parkinson’s and diabetes.
Guidelines indicate care practitioners should work in partnership with the person, developing goals in a collaborative way, including gaining confidence in tasks such as dressing themselves, (NICE NG74, 2017). Every morning a ‘walk round huddle’ is held where the ward sister or senior nurse in their absence, Frailty Nurse Consultant, discharge co-ordinator and a member of the therapy team discusses each patient at their bedside. This includes the patient in discussions and decision making regarding their reablement and rehabilitation needs. Daily goals are agreed with patients and families and written up on a whiteboard above their bed. Patients are encouraged to get out of bed for meals, wash in bathrooms not at the bedside and to get dressed daily. In addition, monthly ‘Afternoon tea with Sister’ events are held on the ward involving Suffolk Family Carers, recognising the importance of nutrition and hydration needs. We also have a relative’s kitchen for refreshments, entirely funded by donations, so they can share drink times/meal times with their loved ones.
NICE recommends a muscle-strengthening and balance programme including an exercise component, (NICE CG161, 2013). A static cycle was purchased for the ward which patients can use with arms or legs, to help maintain muscle strength and encourage early mobilisation. We also purchased activities for patients, introduced social dining as an extra dimension to reablement and purchased slippers to assist patients to walk safely and patient pedometers.
Initially there was resistance from staff, most of the time patients were happy to get dressed but some staff continued to wash patients in beds and keep gowns on. It was a long process to implement a change in attitudes and to motivate patients, particularly older patients. We found that the patient’s perception of their hospital journey was traditionally one where they were cared for, rather than being pushed to maintain independence.
The total project cost for buying in additional equipment was approximately £400, funded by donations made to the ward by patients and relatives, with no additional costs for staffing. Beverage supplies for the patient’s kitchen are funded by ongoing donations.
Key findings
The aims of the project were to recognise frailty and prevent deconditioning to reduce the length of stay for patients on the ward and improve patient wellbeing. Subsequently improving patient flow and reducing the annual costs for admissions, mortality rates and the involvement of other services upon discharge.
The average length of stay before the project was implemented was 8.4 days at a typical cost of £162 per day, (excluding the wards share of overhead costs, medical staff costs, pathology and imaging costs). During the first year of implementation, the average length of stay was reduced to 6.7 days. Furthermore, we saw an increase in function for patients, enabling them to return to their usual residence with less intervention from other services upon return.
Our Ipswich Hospital User Group (IHUG) colleagues are regularly on the ward chatting to patients and feeding back to us as to whether patients feel their needs are being met and if they have any issues or concerns with their progress. Our complaints are also reduced because we are walking round daily addressing patient’s concerns in our huddle by the bedside.
“I have never been on a ward where every one of the staff pushes you to get up and walk and be more independent, we all look better in our room”
“Great to know at the beginning of the day so I can make a start and not worry about what to do, lovely staff”
“It is good that my family can see my board as I sometimes forget and they remind me”
Since implementation, relationships have been built and improved with IHUG, Suffolk Family Carers and chaplains and there is significant improvement in the recognition and understanding of frailty across all staff. We continue to see a deep change of culture on the ward amongst staff as attitudes change and feedback from our patients to date has been very positive, despite initial resistance, with staff committing to personal reablement pledges.
“Having nursed younger people who have become deconditioned after only a few days in bed, it has made me realise how vital it is with elderly patients to ensure that they are assisted to “get up and dressed” as much as possible - Lavenham Ward Sister
Suggestions continue to be made by staff, resulting in small but significant changes, for example moving clocks to enable patients to see the time from their bed space and purchasing large digital clocks for the visually impaired.
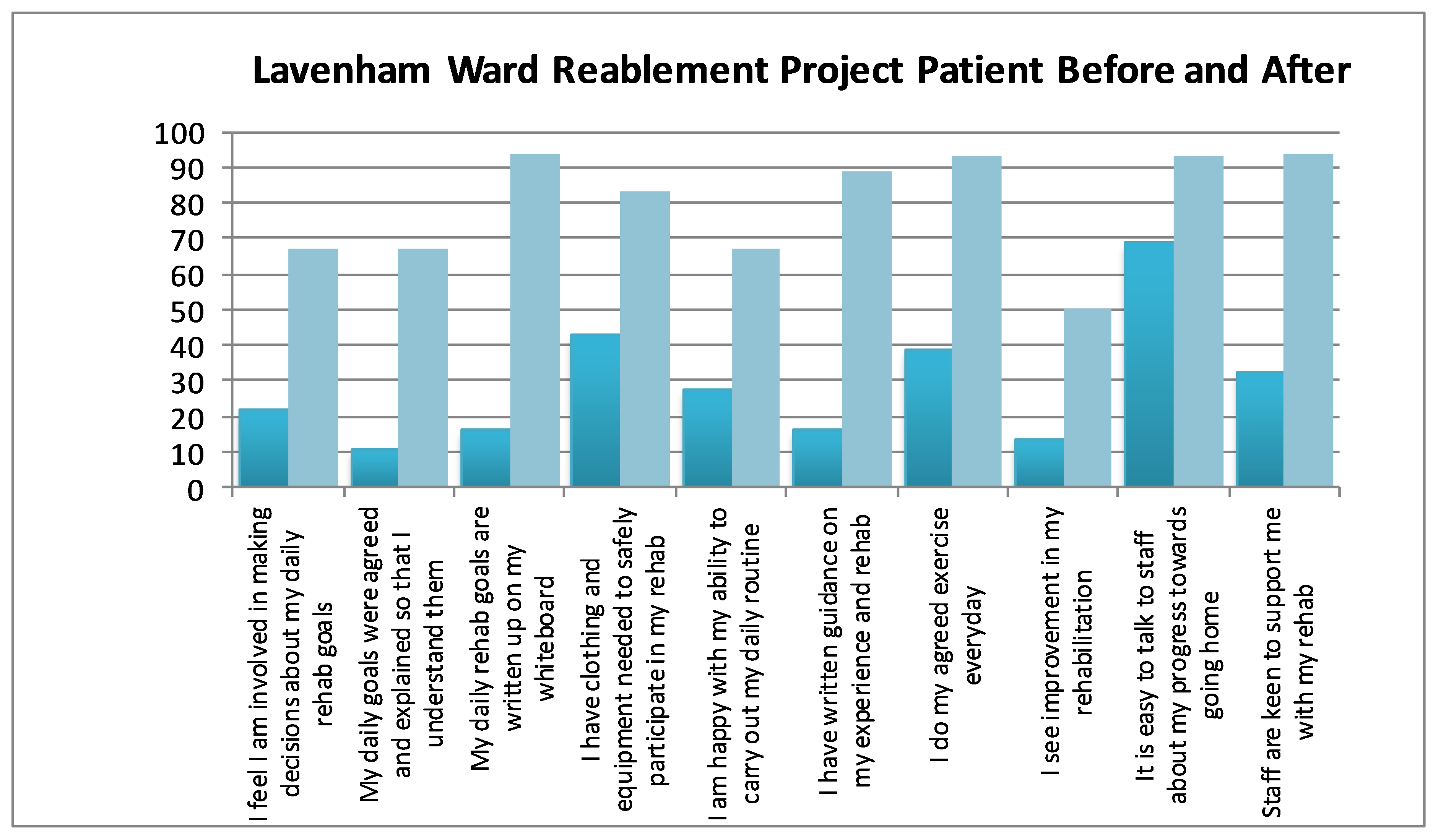
To test the effectiveness of our changes, we re-audited the initial criteria from the short patient survey with very positive results. As a team we were amazed to see how the simple changes we had put in place had made such a difference, (Figure 2).
Figure 2: Re-audit results of the short patient survey before and after the project was implemented
Key learning points
Lavenham Ward is now recognised as a Champion ward and the Trust is rolling out reablement training across all wards in Ipswich Hospital. The Reablement Training Programme will become part of the Trust’s mandatory training and will be included in the Staff Induction Programme.
The key things that have been learnt during this project are that early engagement and ongoing training for staff are paramount to maintain standards and change overall attitudes. Patients are often pushed to maintain independence much quicker than they would like to and some have showed great resistance to change so it is important all staff are able to promote the right message and the reasons why exercise and reablement are so important. Staff still need regular reminding and encouraging to continue the reablement work that is now so vital to our patients. Although we have had a slight increase in the number of falls on the ward since the reablement project began, the level of harm hasn’t increased.
For wards that do not have this kind of service in place we would suggest ensuring daily goals and exercise plans are simple to follow and that the patient agrees with the goals made. We found that the daily beside huddle has been the best way to ensure this happens. Having goals written up on the patent’s whiteboard makes a huge difference to the successful completion of tasks and alongside the physio team, we are currently creating a more personalised paper based exercise and daily goal book.
Implementation of group activities and social dining where patients dine together on the ward around a central table has also been a positive success. Not only in getting patients up and about, but also in improving hydration and nutrition needs. Furthermore, an improvement has been seen in their mental wellbeing and general happiness by the nature of socialising, conversing and laughing with others.
As a team, we know we still have improvements to make to End of Life care in particular to ensure every patient achieves their preferred place of care and preferred place of death. However, we have had families who have been offered hospice or nursing home options, but they feel that the quality of care has been such that they are best placed with us. It is fantastic to reflect on what has been achieved since we have implemented this project and we know that ultimately our patients and their carers experience on our ward will be improved now and in the future.