12 patients admitted for various orthopaedic implant surgeries over a time period from January 2018 to August 2019 developed deep sited surgical wound infections. Initially identified by submission of 5 Datix’s (incident reporting system) by the Surgical Nurse Practitioner.
After the review of cases this number grew to 12, prompting a serious investigation. The identification of these cases also suggested the organisation would have been an outlier, with an surgical site infection (SSI) rate above the national average. From this investigation, enhanced microbiological testing and the involvement of the multi-disciplinary team (MDT) it was identified that the cases weren’t linked and detailed review excluded some of the cases as they did not fit the SSI criteria.
However, through undertaking this review through a quality improvement process and using the One Together framework for assessment, measures were implemented to improve the patient experience and safety, through compliance with NICE guidance NG125.
Example
Aims and objectives
The aim was to improve MDT involvement in the review of suspected surgical site infections and through measuring current practice against NG125, using the One Together framework improve patient safety by improving compliance with best practice and reducing the risk of a surgical site infection for patients undergoing joint replacement surgery.
Reasons for implementing your project
Prior to this work mandatory SSI data figures were collected and feedback to the trauma and orthopaedic directorate and improvements would be made by individual practitioners.
By bringing all relevant teams together it has allowed more detailed quality improvement to take place with clear shared learning through a structured process. For patients it has meant that the care they receive through the surgical directorate and theatre has been brought in line with best practice and NICE guidelines.
This is safer care for over 1000 patients a year, figures taken from 2018/19 where 504 hip replacements and 526 knee replacements took place at Worcester Royal Hospitals NHS Trust. Although mandatory SSI data is not submitted for all quarters to PHE the Trust has implemented continuous SSI surveillance following this work.
How did you implement the project
Following the identification of patients who had joint surgery having a staphylococcal infection an MDT serious investigation review was arranged.
From the review a number of actions were identified. One of the actions was to send the patient samples for further testing and this revealed that they were not linked.
Another was to undertake the One Together framework assessment to identify a baseline of where the current patient pathway through joint surgery sat against best practice guidelines, (NG125).
The baseline showed that all 14 elements of the assessment required improvement. This work was led by the theatre team with support from Infection prevention and control. In addition, the review facilitated a full review of the theatre environment and the Estates team worked to ensure that these met the required standards.
Key findings
The aims and objectives have been achieved. This was a multi-disciplinary approach to establish quickly and effectively if there was an underlying problem.
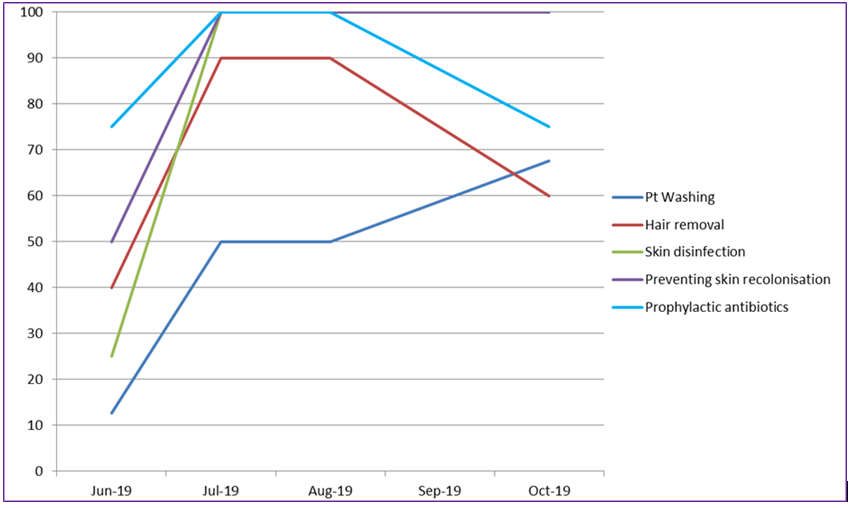
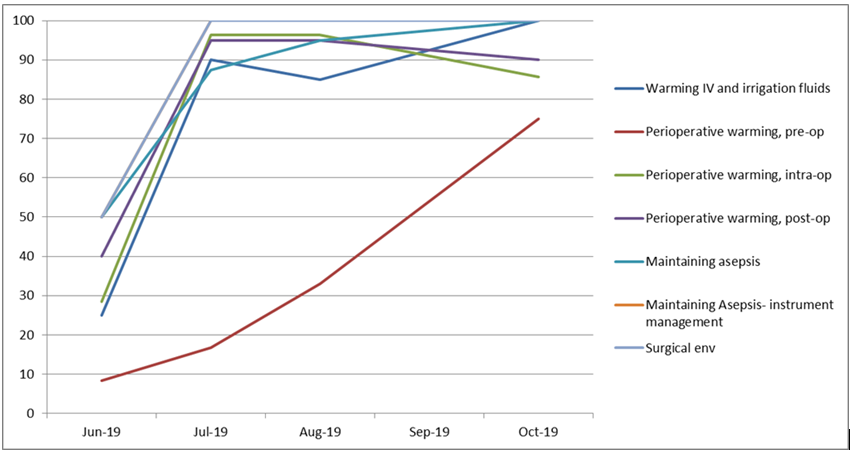
The approach proved a positive experience for those involved and has created many changes that may have perhaps been overlooked without this level of scrutiny. By utilising the One Together assessments clear improvement with compliance with NG125 can be seen, (Chart 1 and 2).
Chart 1)
Chart 2)
The theatre team have taken ownership of maintaining compliance with NG125 and have updated local policies to bring them in line with best practice, they continue to use the One together assessment tool to give compliance assurance.
Whilst we are confident there were no issues with the trust surgical site infection rates, we are also now confident that processes are in place decreasing the potential for infection to patients even further.
Key learning points
Gaining the involvement of all involved has supported a positive change with each team controlling their own area of expertise/practice.
This has led to a cohesive improvement that would not have had such an impact if it had been carried out in isolation. Furthermore, there have been added benefits in that it has given an opportunity for several staff to gain familiarity with Improvement and governance processes.