Women can develop mental ill health for the first time during pregnancy, and pre-existing mental health conditions can get worse in the perinatal period. Perinatal mental health problems affect up to 20% of women with an estimated cost of almost £10,000 per birth.
Mental health problems during the perinatal period can frequently go unrecognised and untreated, with some women not seeking help because of fear of stigma, or fear of intervention by social services. If left untreated, perinatal mental health problems can have significant and long-lasting effects on the woman and her family, as well as on children’s emotional, social and cognitive development. NICE has produced guidance to reduce the risk of mental illness during pregnancy and reduce harm for both mother and child.
Perinatal mental health problems are those which occur during pregnancy or in the first year following the birth of a child.
Emotional wellbeing checks ensure women are monitored and supported to maintain good mental health.
Perinatal mental health services
Access to specialist multidisciplinary perinatal community services and inpatient psychiatric mother and baby units can help to ensure that the most appropriate assessment, monitoring and treatment is provided. The NICE quality standard and guideline on antenatal and postnatal mental health state that these services should be available to support women with a mental health problem during pregnancy or the postnatal period. They are currently only found in a minority of providers, as they require the redesign of services.
The Five Year Forward View for Mental Health made the commitment to support at least 30,000 more women each year to access evidence-based specialist mental health care during the perinatal period by 2020/21. To provide this care NHS England have developed a five-year national transformation programme to build capacity and capability in specialist perinatal mental health services.
As part of the transformation of these services, in May 2018 the National Collaborating Centre for Mental Health worked with NICE to publish the perinatal mental health care pathways. This provides services with evidence on what works in perinatal mental health care, as well as case studies describing how areas are starting to make this a reality.
These services include community perinatal mental health teams which have been included in the national transformation programme. In 2017, 71% of sites had access to a community perinatal mental health team, as shown in the National Maternity and Perinatal Audit.
In April 2019, NHS England announced the roll out of specialist perinatal community services across the whole of England in line with commitments to transform services from the NHS Long Term Plan.
Shared learning example
Using NICE guidance for antenatal and postnatal mental health to improve the quality of NHS services working with women during the perinatal period
Thames Valley Perinatal Mental Health (PMH) Network designed an online self-assessment tool for NHS services working with women with or at risk of developing perinatal mental health problems. This enables maternity, health visiting, secondary care mental health and Improving Access to Psychological Therapies (IAPT) services to benchmark performance against NICE guidance and Royal College of Psychiatrists PMH workforce standards. The tool has been endorsed by NICE and is being implemented across NHS England south regions.
Results are available on a live dashboard and can be viewed at regional, Local Maternity System, CCG and service level. The tool identifies good practice and gaps in service provision and data collection; guiding service development tailored to the local service landscape and demand, mapping performance progress over time.
I have an amazing local perinatal mental health team. I had a community psychiatric nurse who I had regular sessions with during pregnancy and after my second son was born. When I had a mental health crisis, she was at my house within 45 minutes and my psychiatrist had prescribed my medication so I could start it that day. I owe them so much. Every mother and family should have access to care like that, it would improve so many lives.
Emotional wellbeing
Asking women about their emotional wellbeing provides an opportunity to identify potential mental health problems. It also gives women an opportunity to talk about any concerns they might have, such as fears around childbirth, multiple pregnancy, or past experiences, such as loss of a child or traumatic childbirth. This enables healthcare professionals to provide appropriate support and signpost to services as required.
The NICE quality standard on antenatal and postnatal mental health highlights that women should be asked about their emotional wellbeing at each routine antenatal and postnatal contact. The NICE guideline on postnatal care up to 8 weeks after birth recommends that, at each postnatal contact, women should be asked about their emotional wellbeing, what family and social support they have and their usual coping strategies for dealing with day‑to‑day matters.
The Care Quality Commission surveyed women about their experience of maternity care, with over 90% of eligible women asked.
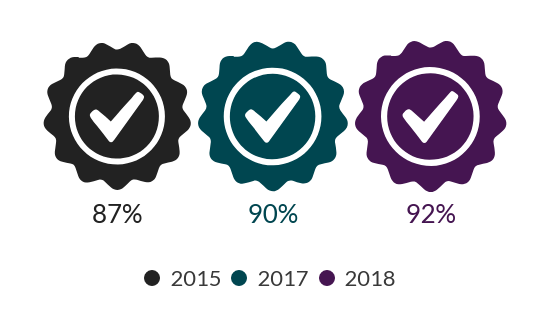
According to the survey there has been an increase in midwives routinely asking about emotional wellbeing at antenatal check-ups.
Between 2015 and 2018 more midwives are carrying out emotional wellbeing checks at antenatal check-ups
Emotional wellbeing checks at antenatal check-ups
The survey also shows that emotional wellbeing checks continue to be undertaken for most women after childbirth by a midwife or health visitor.
Nearly all women have their emotional wellbeing checked after birth
Emotional wellbeing checks after birth
Most mothers were also told who to contact if they needed advice about any emotional changes they might experience after birth.
Between 2015 and 2018 there was a slight increase in the proportion of mothers who were told who to contact for emotional support after birth
Mothers told who to contact for emotional support after birth
Encouragingly, additional data from the NHS Safety Thermometer showed that in 2018 only 2.1% of women reported being left alone at a time that worried them in a hospital, midwife led unit or community setting.