24 May 2016
NICE recommends three diabetes treatments
NICE has published final guidance recommending three drugs for treating type 2 diabetes.
The three drugs can all be used on their own if a person can’t use metformin or other specific drugs[1], and diet and exercise alone isn’t controlling their blood glucose levels.
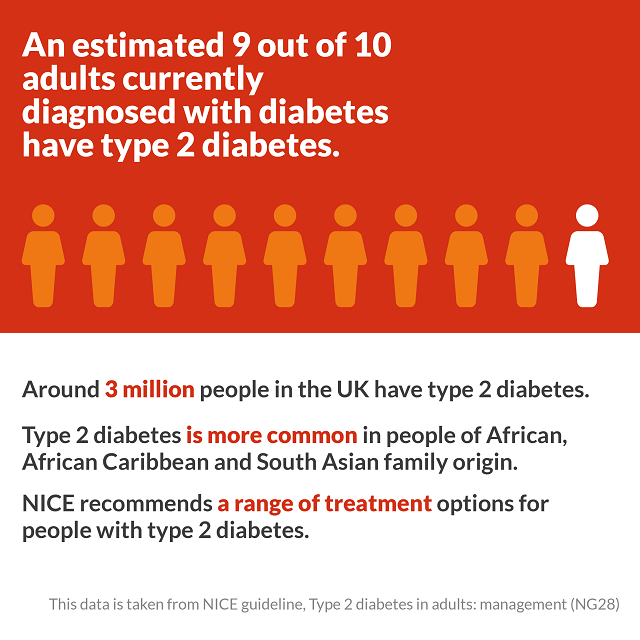
Around 3 million people in the UK have type 2 diabetes. An estimated 31,000 people may be eligible for the three recommended treatments: canagliflozin (Invokana), dapagliflozin (Forxiga) and empagliflozin (Jardiance). The cost of a course of treatment over one year with each drug is around £475.
Professor Carole Longson, director of the NICE Centre for Health Technology Evaluation, said: “Type 2 diabetes is long-term condition that has a serious impact on people who live with it, and the treatments given should be tailored for the individual.
“For many people whose blood glucose levels aren’t controlled by diet and exercise alone, metformin is the first drug treatment that they’ll be offered. But some people may experience nausea and diarrhoea, and they may not be able to take it if they have kidney damage. For people who can’t take a sulfonylurea or pioglitazone, then the three drugs recommended in this guidance can be considered. This is as an alternative to the separate group of drugs called dipeptidyl peptidase-4 (DPP-4) inhibitors.
“The committee agreed that people with diabetes and their clinicians would value having an additional treatment option to help manage their type 2 diabetes – which this positive guidance provides.”
Adults currently receiving NHS treatment with canagliflozin, dapagliflozin or empagliflozin on its own that is not recommended for them in this guidance should be able to continue treatment until they and their NHS clinician consider it appropriate to stop.
Ends
[1] Sulfonylurea or pioglitazone.
About the guidance
1. The guidance, ‘Canagliflozin, dapagliflozin and empagliflozin as monotherapies for treating type 2 diabetes’ is available from the NICE website from Weds 25 May 2016 at www.nice.org.uk/ta390.
2. The three drugs considered in this appraisal are: canagliflozin (Invokana, Janssen), dapagliflozin (Forxiga, AstraZeneca) and empagliflozin (Jardiance, Boehringer Ingelheim and Lilly UK). The drugs are all selective sodium-glucose cotransporter 2 (SGLT-2) inhibitors, which block the reabsorption of glucose in the kidneys and promote excretion of excess glucose in the urine.
3. The recommendations are:
a) Canagliflozin, dapagliflozin and empagliflozin as monotherapies are recommended as options for treating type 2 diabetes in adults for whom metformin is contraindicated or not tolerated and when diet and exercise alone do not provide adequate glycaemic control, only if:
• a dipeptidyl peptidase-4 (DPP-4) inhibitor would otherwise be prescribed and
• a sulfonylurea or pioglitazone is not appropriate.
b) Adults whose treatment with canagliflozin, dapagliflozin or empagliflozin as monotherapy is not recommended in this NICE guidance, but was started within the NHS before this guidance was published, should be able to continue treatment until they and their NHS clinician consider it appropriate to stop
4. The recommended starting dosage of canagliflozin is 100 mg orally once daily, and in certain circumstances the dose can be increased to 300mg once daily. The price of canagliflozin is £39.20 for a 30-tablet pack of 100 mg or 300 mg tablets.
The recommended dosage is 10 mg dapagliflozin orally once daily for monotherapy. The list price of dapagliflozin is £36.59 for a 28-tablet pack of 5 mg or 10 mg tablets.
The recommended starting dosage of empagliflozin is 10 mg orally once daily for monotherapy, and the dose can be increased to a maximum of 25 mg daily in certain circumstances. The list price of empagliflozin is £36.59 for a 28-tablet pack of 10 mg or 25 mg tablets.
For all three drugs, list prices exclude VAT and costs may vary in different settings because of negotiated procurement discounts.
5. The three drugs were cost effective compared with DPP-4 inhibitors (also called gliptins) incremental cost effectiveness ratio (ICERs) of less than £29,300 per quality-adjusted life year (QALY) gained. However, they were not cost effective compared with pioglitazone (more than £52,400 per QALY gained) and sulfonylureas (over £71,000 per QALY gained). When the three drugs were compared with each other, the committee agreed that the clinical evidence and cost data (all tablets cost the same and had the same frequency of administration) did not support any differences between them.
Therefore the committee concluded that canagliflozin, dapagliflozin and empagliflozin as monotherapy are a cost-effective use of NHS resources for treating type 2 diabetes in adults for whom metformin is contraindicated or not tolerated, and when diet and exercise alone do not provide adequate glycaemic control, but only when pioglitazone or sulfonylureas are not appropriate treatment options.
6. There are almost 3.5 million people who have been diagnosed with diabetes in the UK (Diabetes UK, Nov 2015). It is estimated that about 90% of adults currently diagnosed with diabetes have type 2 diabetes. A person with type 2 diabetes has too much glucose (sugar) in their blood. This can either be because their body doesn’t produce enough insulin – the hormone which controls the amount of glucose in blood – or their body doesn’t use insulin effectively. If blood glucose levels are not managed effectively it causes tissue damage which can result in blindness, kidney failure, foot ulcers which can lead to amputation, and also premature heart disease, stroke and death. Type 2 diabetes is more common in people of African, African Caribbean and South Asian family origin.
About NICE
The National Institute for Health and Care Excellence (NICE) is the independent body responsible for driving improvement and excellence in the health and social care system. We develop guidance, standards and information on high-quality health and social care. We also advise on ways to promote healthy living and prevent ill health.
Our aim is to help practitioners deliver the best possible care and give people the most effective treatments, which are based on the most up-to-date evidence and provide value for money, in order to reduce inequalities and variation.
Our products and resources are produced for the NHS, local authorities, care providers, charities, and anyone who has a responsibility for commissioning or providing healthcare, public health or social care services.
To find out more about what we do, visit our website:www.nice.org.uk and follow us on Twitter: @NICEComms.