Embedded within a cross-sector system approach, we describe the development and application of a general practice quality improvement package, underpinned by NICE Quality Standard QS28 for hypertension in adults. The package includes consultation templates, protocol, patient information and a dashboard of indicators to monitor progress and performance to the Quality Standard. Hypertension is referred to as ‘high blood pressure (BP)’, as it is throughout the C&M BP work, to reduce language barriers to cross-sector partnership working.
Cheshire and Merseyside’s (C&M) system leadership approach to high BP aims to embed a widespread culture of integrated cross-sector working in which responsibility for action is distributed beyond just health partners. A range of partners including: public health, health, NICE, local authority, voluntary sector and other partners formed a sub-regional Partnership Board to co-craft and oversee implementation of a cross-sector blood pressure strategy.
- Hypertension in adults (QS28)
Example
Aims and objectives
The C&M BP strategy vision is that our communities will have the best possible blood pressure. This will improve population health and wellbeing by reducing medical complications such as heart disease, stroke, chronic kidney disease and dementia. As a result it will also contribute to improved sustainability of health and care services.
As part of a cross-sector strategy, the quality improvement package aims to:
- Reduce unwarranted practice-level variation in management of BP across the region.
- Enable general practice to achieve best practice in BP care and management to the NICE Quality Standard without additional burden on resources.
- Use practice-level benchmarking data to highlight the need for local quality improvement interventions and to monitor progress.
The package provides easy access to a NICE standard compliant nurse-led consultation, and maximises signposting to BP medication reviews in community pharmacies, self-help and lifestyle interventions in the community.
We aim to demonstrate improved performance against the NICE hypertension quality standard (QS28), and when the quality improvement package is widely adopted across C&M we aspire to achieve a 1% increase per annum in known BP patients who are treated to <150/90mmHg, and a 10% reduction per annum in practice-level variation for the same measure.
Reasons for implementing your project
Cheshire and Merseyside has a population of approximately 2.4m, of which approximately 625,000 people are thought to be affected by high blood pressure (BP). Almost half of this number unaware they are affected, and there is unwarranted variation in care of known high BP patients. Tackling high BP offers considerable scope to reduce medical complications such as heart attacks, stroke and dementia, and to make substantial financial savings across the health economy. Action is needed to improve prevention, detection and management of the condition.
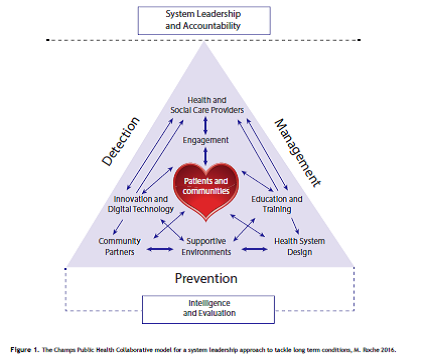
High blood pressure (BP) was identified as one of a number of priorities for collaborative action by the C&M Directors of Public Health in 2014. This marked the beginning of a cultural change across the sub-region. In 2015 the C&M cross-sector BP Partnership Board was established, and the following year the Board launched a five year strategy to tackle high BP ‘Saving Lives: Reducing the pressure’. The strategy sets out 10 inter-related objectives, as represented schematically below:
When the NHS Sustainability and Transformation Plans (STPs) were announced later that year, high BP was included as one of three C&M prevention priorities. An ambitious ‘invest to save’ action plan for high BP was developed, and the C&M BP Board subsequently reported to the C&M [STP] Prevention Board. The BP quality improvement package was developed to meet strategic objectives and also as a priority high BP STP deliverable.
NICE guidelines and quality standards set out evidence-based best practice for management of high BP. A baseline assessment in 2017 demonstrated a patchy knowledge of practice-level performance against NICE hypertension guidelines across C&M, and where local audits were available, these highlighted scope to improve.
Improving performance against NICE guidelines can contribute to closing the 3 ‘gaps’ as set out in the STP: ‘Care and Quality’, ‘Health and Wellbeing’, and ‘Finance and Efficiency’. It is estimated that if all C&M GP practices performed as well as the 75th best percentile for managing known BP patients, 183 strokes, 118 heart attacks, 256 cases of heart failure, 96 deaths could be prevented over 5 years. Indeed, if achieved alongside a 5% to 15% increase in diagnosis, economic modelling estimates that C&M could see a net financial benefit of between £7m and £8.2m in five years (discounted), based on investment of around £500k p.a. across C&M, including support for the quality improvement package described.
How did you implement the project
In 2015 C&M was successful in a £100k Health Education England (HEE) bid to develop a local BP education and training programme for partners including general practice. This funded (amongst other things) protected PH consultant time to lead and support early development and piloting of the quality improvement package.
The package was built on insight from primary care workshops; a NICE-led online survey, and NICE-led “Ketso” focus group. GPs and nursing staff identified the need to focus on practice nurses and healthcare assistants (who conduct most BP checks). The need for accessible consultation templates, protocols, training and audit-support were also highlighted. Information for patients was seen as important to support self-care.
The package was co-developed and implemented by British Heart Foundation working with a local practice, and with support from the Champs public health collaborative. It is aligned to NICE hypertension guidance and quality standard, and includes:
- EMIS Web-based consultation templates for new and existing patients
- ‘Gold standard’ practice protocol
- Practice-level data dashboard/ audit tool
- Patient information prescription
- Training.
Some screenshots from the resource can be found here.
Implementation was gradual, starting with a small number of early adopting practices across the sub-region (aiming for at least one per CCG). These received one to one support from the BHF team. Opportunities to build capacity to enable scaling-up across C&M are being explored with NHS England (C&M) through the C&M General Practice Nursing Collaborative.
Some key challenges included:
- Identifying technical expertise to build the audit tool/dashboard, ensuring information governance-compliance and creating a ‘live’ run as opposed to using less timely data retrieval and return.
- Dependence on a system leadership approach, networking and to a large extent good will to develop the package meant timeframes had to be adaptable.
- Translation of the EMIS-compatible templates for other IT systems, and a solution for centrally- coordinating template updates.
Partners also included NICE (strategic and operational support), NHS England/ C&M General Practice Nursing Collaborative (implementation support and capacity-building), Public Health England (data role), Sefton, Wirral and Liverpool CCGs (dashboard development), Blundellsands practice (co-development and piloting).
Key findings
Implementation of the package is at an early stage, but as at January 2018, four early adopting practices have been established across three CCGs, with an aim of establishing at least one early adopting site per CCG.
A retrospective baseline audit of performance against the NICE Hypertension Quality Standard will be carried out for early adopter sites this month.
Initial feedback from early adopting sites after a couple of months of using the package indicates:
- The template /protocol identified inconsistencies in the practice process of hypertension management.
- Nursing staff really liked the templates, particularly for newly diagnosed patients.
- A lack of confidence and educational need around hypertension reviews.
An interim evaluation is planned in the spring, looking at changes in practice-level performance against the NICE Hypertension Quality Standard, and also more detailed qualitative feedback from practice staff in terms of what went well, and what could be improved. This will inform refinement of the package before scaling up availability.
Performance against the NICE Quality Standard for hypertension will be reviewed at least annually as part of a more comprehensive monitoring of impact of the BP strategy and progress with BP STP (now Health and Care Partnership) key performance indicators.
Key learning points
The content of the package is expected to cover the aims we originally described, and it links to a number of other BP work-streams developing in C&M e.g. BP testing outside of general practice, medicine optimisation in community pharmacy, and Making Every Contact Count.
Before and after audits in early adopter practices, and the interim evaluation planned for spring will give greater insight into the utility and impact of the package. Outputs of the package will also contribute to key deliverables within both the C&M BP strategy and the C&M Five Year Forward View action plan.
When we started the programme, we pictured a more traditional ‘education and training’ approach for general practice. However, local insight work informed us that the key stakeholders wanted and needed something more supportive and practical than traditional teaching sessions in isolation. This highlights the importance of keeping an open mind, listening to what is needed and responding accordingly. As a result we have a practical quality improvement package that addresses needs in general practice.
Identifying capacity and resource to roll-out any initiative at scale is a challenge at present, and the acceptability of any change in practice increases with co-production and peer to peer endorsement. Encouraging a friendly but competitive spirit across practices to incentivise performance was important to success. A sector-led improvement approach was achieved through a combination of benchmarking data and shared learning by early adopting practices.
Buy-in from practice nursing teams (as well as GPs) is important to the successful implementation of the package. Practice nurses and health care assistants are often the members of a primary care team who conduct BP consultations. Protocols and templates that allow quick, logical but evidenced collection of information are highly valued by practice nursing teams.
The package could be adapted or expanded to include a range of other long term conditions.
Contact details
Health Education England funding supported development of a C&M BP education and training package. The British Heart Foundation committed staff time and sponsored a C&M BP event, ‘The Big Pledge’ 2017.