A quality improvement audit at a GP practice (Newton Medical Centre) in line with the NICE guideline [NG150] Supporting adult carers.
It aims to improve the lives of carers by helping health and social care practitioners identify people who are caring for someone and give them the right information and support. It covers carers’ assessments, practical, emotional and social support and training, and support for carers providing end of life care.
Our quality improvement project specifically relates to section 1.2 of the guidance covering identifying carers, 1.3 around assessing their needs and recommendations in section 1.5-7 around offering them support and practical help.
- Supporting adult carers (NG150)
Example
Aims and objectives
- To validate the register of carers in the practice - NICE guideline [NG150] recommendations 1.2.1-5
- To assess the needs (physical, psychological, emotional, financial etc.) of the carers
- To assess the impact of COVID-19 on their role specifically
- To offer practical help where indicated and signpost them where appropriate
Reasons for implementing your project
The roles and responsibilities of the unpaid carer were traditionally overlooked by the wider health care system in the UK. However, in May 2014, NHS England published an official framework that highlighted the lack of support and a need for better recognition of carers. It stated that carers should be considered a hugely important asset to the NHS and therefore deserve respect and support from clinicians. This ‘Commitment to Carers’ documentation set out eight priorities to improve the experiences and lives of care givers.
The fifth priority focused specifically on the primary care setting; supporting GPs to better identify carers and enhance the services available to them. These recommendations echoed much of the information presented in the guidance published by the RCGP ‘Commissioning for Carers’ in 2013, a document that contained many examples of the challenges faced by those with lived experience of unpaid caring. Although personal anecdotes can be perceived as overly emotive, in this documentation, they enhance the readers’ recognition of the need for additional support for carers. The change in consultation style due to the COVID-19 pandemic has resulted in fewer patients, and therefore carers, attending practices for consultations. As a result, there are fewer opportunities to meet carers in person which could result in the oversight of many concerns or problems. Furthermore, to mitigate risk in the early months of the pandemic, the government advised extremely vulnerable members of the population shield from the rest of society. Many carers also had to isolate and would not have had the opportunity to attend face-to-face appointments for themselves. The most contemporary evidence suggests that isolation, loneliness and dramatic change has resulted in a stark rise in mental health problems and this could be affecting carers. GPs must therefore find novel methods to reach out to carers registered with their practice to ensure that they feel supported and safe.
The recently discovered SARS-CoV-2 virus and resultant COVID-19 pandemic created many challenges for both the UK healthcare system and wider society. Social distancing, hand hygiene and the wearing of facemasks were introduced as a manner of mitigating the pressures on resources (Intensive Care Units and ventilators) while a safe and appropriate vaccination programme is developed.
In the primary care setting, there were additional changes to practice; in March 2020, GPs received specific guidance from NHS England that led to the replacement of many traditional ‘face to face’ consultations with telephone or video calls. This decrease in footfall within practices has resulted in fewer interactions between GPs and carers who would normally attend appointments to support their dependents.
It is possible therefore that during this novel pandemic the changing needs of carers are being overlooked by clinicians, which could lead to detrimental outcomes within this highly valued cohort. This audit aims to assess the impacts of the pandemic on a cohort of carers registered with this practice and offer practical support.
How did you implement the project
This project aimed to contact all those registered as carers at the Newton Medical Centre in September and October 2020. Data collection was carried out via telephone calls over a four-week period.
An initial search of the EMIS database provided a list of individuals registered at the practice who identified as carers. This list was then searched to remove all individuals reported to no longer be caring for a dependent. Medical students attempted to telephone all 199 remaining individuals to gather data.
A timeline was agreed by those involved in data collection and analysis to ensure that outcomes from the project are reached in a timely manner. Each carer received a telephone call to ascertain data regarding their current caring status and any concerns or issues they have faced due to the COVID-19 pandemic. The carers’ responses highlighted the areas to focus on for quality improvement work that led to the implementation of changes at the practice in October 2020.
Key findings
Of the 199 individuals called, 139 patients answered the call and engaged with the survey. Of the 139 people engaged with, 92 were currently carers and 47 were no longer carers and their records have been updated.
Of those currently caring, 54 described specific impacts of the COVID-19 pandemic on carers as below (themed):
- Social isolation - 27
- Decline in mental health - 15
- Difficulties accessing appointments - 6
- Lack of support groups - 3
- Lack of respite - 1
- Fear of COVID-19 - 1
- Physical health concerns - 1
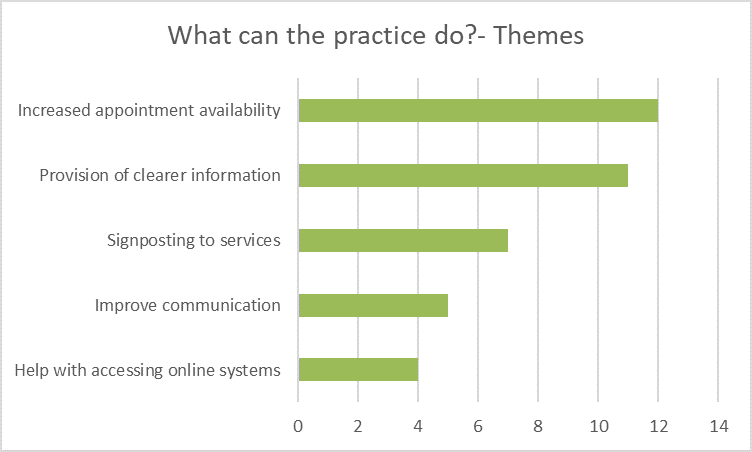
30 carers had suggestions for the improvement of services at the practice (see attached report for further details).
Themes from the qualitative responses and concerns were discussed in a clinical meeting and actions to address these issues have been implemented as part of quality improvement activities within the practice. Letters with relevant information were sent out to the carers.
Quality improvement is integral to progressive practice and focuses on making small scale interventions to drive change in current systems and improve patient experience. We have carried out these straightforward actions on the grounds of results from this audit and updated the patient records (General Medical Council guidance recommends that clinicians maintain accurate and up to date records).
The 47 individuals contacted that are no longer carers, have had their EMIS records updated accordingly. This will prevent repetitive and potentially distressing conversations about the deaths of dependents, thus, improving the holistic approach towards the care of patients registered with the practice.
Key learning points
Logistical issues raised, such as the need for increased access to appointments and better communication from the practice, were fed into a clinical meeting to facilitate appropriate interventions that align to national guidance.
There was an apparent misconception that GPs were interacting and caring for fewer patients as a result of the pandemic. This is incorrect. Practices have merely altered consultation methods where appropriate and in line with contemporary guidance. The 139 carers reached by telephone were reminded that they can still seek support and advice should they require it. Correspondence has been sent to thank those who took part in the survey and highlight the positive changes made by the practice as a result of their valued responses.
The letters provided information regarding the annual influenza vaccination scheme, access via e-consultation, telephone advice calls, limited face-to-face after triage by clinicians and support groups that have continued to help carers during the pandemic. Carers UK is an example of such support groups This charity is dedicated to giving expert advice and information to care givers. They are also passionate about connecting individuals to create a network of carers to support one another and share experiences.
The latter may provide comfort for those carers who disclosed struggles relating to the social isolation brought about by the pandemic.