Kent Surrey and Sussex (KSS) Academic Health Science Network (AHSN) Alliance for Atrial Fibrillation (AF) aims to reduce the number of people dying or disabled by AF-related stroke, by increasing the detection of patients in AF and optimising the use of anticoagulants in line with NICE AF guidance (NG196).
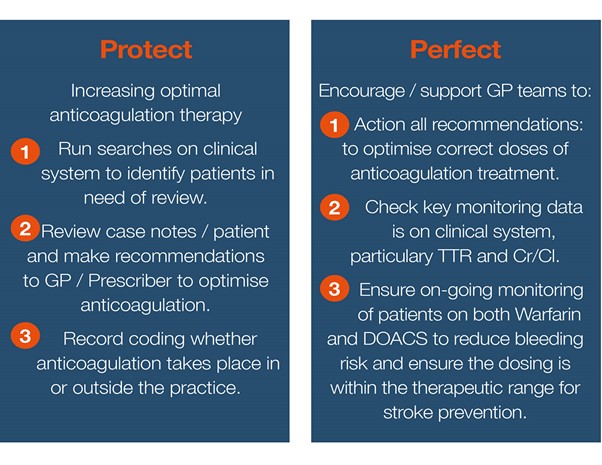
Implementing a robust package of AF tools and resources to GP practices, in addition upskilling clinical pharmacists through education and mentorship to support them to deliver best practice and recommendations from NICE NG196 guidance in the 3 key focus areas of Detect – checking for irregular pulse, Protect – reviewing and anticoagulating, Perfect – optimising treatment and monitoring
This shared learning case study will focus on the protect and perfect aspects of the programme.
This example was originally submitted to demonstrate implementation of NICE CG180. This guidance has been updated and replaced bynew guideline NG196. The example has been reviewed and continues to align generally with the updated guidance which should be referred to if replicating any aspect of this example.
Example
Aims and objectives
The aim of the initiative was to avert strokes and deaths through the implementation of a range of tools and resources to support the clinical teams. We were able to measure the impact in real-time using a standardised and measurable approach of computerised interrogation of the GP database to identify known AF patients at high risk of having an AF-related stroke and help specialist pharmacists identify patients in need of review. KSS AHSN co-ordinated the approach and Oberoi Service Implementation Managers visited each surgery to set-up the clinical systems and train the allocated Pharmacist on the systematic approach to facilitate their work.
This tool assisted GP practices with the complete management of patients with AF. In real-time at the press of a button it generates lists of diagnosed AF patients where clinical intervention is missing along with opportunistic prompts (aligned to AF NICE guidance) to ensure known AF patients with missing clinical interventions are captured during consultations. A secure e-portal enables practices to track the level of intervention taking place in their practice as well as benchmarking their performance vs, other participating practices.
The search system in the service proved very useful to the pharmacists, alongside delivering the NHS England virtual clinic atrial fibrillation (AF) Demonstrator Programme. The pharmacists uploaded non-patient identifiable data monthly to the service e-portal to assess the impact of their work on an on-going basis.
The aim in 2020 is to spread the Oberoi SPAF & Case Finding Service further using secured Medical Education Goods Services (MEGs) funding, across a further 100 GP Practices to support in-house practice clinicians to Protect and Protect patients diagnosed with AF on appropriate anticoagulation therapy in line with NICE guidance, thereby delivering on CVD Prevention.
Reasons for implementing your project
East Kent CCGs: Ashford, Canterbury & Coastal, South Kent Coast and Thanet have 17,765 patients coded with a diagnosis of AF on the register (QOF 2017/18)
In East Kent CCGs, the anticoagulation rate was 80.9% (QOF 2017/18 data), the project target is to reach 90% anticoagulation rates by end of 2019/2020. To achieve this target East Kent practices, need to have collectively anticoagulated a further 1,342 known AF patients at high risk of having an AF-related stroke.
KSS AHSN collaborated with East Kent CCGs as key delivery partner to co-ordinate the implementation of NICE AF guidance and the AF package of support in 10 GP practices. The practices were all participating in the NHS England AF Demonstrator Programme and KSS AHSN funded the Oberoi SPAF & Case Finding Service in all 10 practices to support the clinical pharmacists to deliver the work. KSS AHSN also upskilled the pharmacists with education and mentorship programmes, collated the feedback and data findings throughout the project to write up a case study to share learning and impact made on outcomes. As a result of the case study findings the project is now going to be spread to a further 100 GP practices.
AF package of support includes:
Protect: Virtual Anticoagulation Clinic Model (NHSE AF Patient Optimisation Demonstrator Programme).
Perfect: System searches to increase optimal anticoagulation, monitoring and ensure correct coding recorded.
Clinical Audit & Reporting Data: Measured the ongoing impact of detect, protect and perfect at Practice, PCN and CCG level through the Oberoi SPAF & Case Finding Service.
Education: CVD Education Programme for Clinical Pharmacists (quarterly).
Mentorship: CVD drop in Zoom Call for Clinical Pharmacists led by Dr Richard Blakey, KSS AHSN CVD Clinical Lead (weekly).
Resources: Access to a KSS wide CVD online platform to access shared learning, resources and aligned to NICE guidelines. Including: Atrial Fibrillation, Heart Failure, Cardiac Rehabilitation, Cholesterol and Familial Hypercholesterolemia.
National targets set by NHS England in April 2018 to increase anticoagulation rates to 84% by March 2020, were successfully achieved by KSS AHSN Alliance for AF in first year (QOF 2018/19 data).
Kent Surrey Sussex Anticoagulation rates:
82.9% at baseline (QOF 2017/18) rising to 84.6% In 1 year (QOF 2018/19)
How did you implement the project
Engagement of practices was supported and co-ordinated by KSS AHSN and South Kent CCG medicines optimisation teams. Oberoi Service Implementation Managers followed up with the practices and pharmacists to coordinate deployment.
Progress updates were provided to key stakeholders, pharmacists, practices, CCGs and the AHSN from Oberoi Consulting on a periodic basis to communicate the impact being made.
The system that was adopted enabled searches to identify patients with confirmed AF at high risk of having a stroke that sit within the GP system. Along with the opportunistic prompts that alert a clinician during any consultation, if the patient requires a review and intervention, by highlighting issues such as: the patient is at high risk of a stroke but not on any anticoagulation therapy, unstable on their anticoagulation, on the wrong dose of DOAC or missing key elements of monitoring required whilst on anticoagulation.
The super-user’ reports enable primary care networks (PCNs), CCGs and the AHSN to benchmark performance for all participating practices. High level target improvements can easily be tracked on increased anticoagulation rates, perfection of treatment and best practice shared.
To support perfecting anticoagulation, the searches identify whether incorrect doses of Direct Oral Anti-Coagulants (DOACs) are being given, enabling clinicians to correct doses to improve efficacy and reduce potential side effects. For those on Warfarin it extracts which patients have time in therapeutic range (TTR) values in the system and those with a TTR < 65%.
Monthly dynamic reporting is delivered through the e-portal to show the impact being made on Protect and Perfect vs baseline. Reporting is available at practice, PCN and CCG level.
Ambitious targets were set in East Kent of a protection (anticoagulation) rate of a minimum of 90% of the AF high risk population. Perfection of anticoagulation was also high on the agenda to ensure identification of patients with AF who maybe being prescribed sub-optimal warfarin or incorrect dose of DOAC.
The project practice data from the e-portal reports feeds into the wider AF project KSS AHSN quarterly highlight reports for Practices, PCNs / CCGs / STP and the overall project evaluation report.
Key findings
We collated the Oberoi SPAF audit data from 10 practices all with the full package of AF support implemented. All practices had, Virtual Anticoagulation Clinics, Oberoi SPAF and Case Finding Service, access to CVD online platform for shared learning and resources and CVD Mentorship and Education Programmes.
Protect data:
Note: 3 practices data were excluded from Protect data as the Warfarin patients were treated / monitored by a third party and the GP Practice had not coded 8B2K to say anticoagulation takes place outside the practice.

Perfect data:
Perfecting treatment, monitoring patients and recording data is paramount to patient safety, whether anticoagulation takes place within or outside a practice. Dosing can then be amended accordingly. Patient Safety: Perfecting treatment is key to reduce bleeding risk and ensure dosing is within the therapeutic range for both Warfarin and DOACs for stroke prevention.

Patient Safety:
Perfecting treatment is key to reduce bleeding risk and ensure dosing is within the therapeutic range for both Warfarin and DOACs for stroke prevention.
Key learning points
• Embark on this work together as a PCN, involve the whole practice.
• Identify a CVD Clinical Lead at each practice to drive this work forward and upload non-patient identifiable data on the 1st of every month to the Oberoi e-portal (takes 5 mins).
• Focus time on checking there is correct coding on the clinical system for diagnosis, treatment and monitoring of AF patients.
• Correct the coding on the clinical system for mis-coded or missing AF patients
• Check coding on the GP clinical system is added for patients receiving Warfarin treatment/ monitoring from a third party. (code 8B2K to say anticoagulation takes place outside the practice).
• Increase communication between Practice and Anticoagulation Clinics to ensure patients are being safely treated and monitored.
• Check TTR data is recorded on the GP Clinical System for every patient receiving Warfarin Therapy.
• Check all DOAC patients have measurements recorded on the clinical system required for initiating and dosing. These being Weight, Serum Creatinine, Creatinine Clearance (CR/CL) (*CR/CL is a calculation) recorded at baseline and every 6 months. (or at least once a year).
• Ensure patients are optimised on correct doses of warfarin and DOACs to reduce risk of strokes and bleeding side effects.