A vaginal birth is generally recognised as giving the best outcomes for the majority of women and their babies at the end of an uncomplicated pregnancy. However, even after a normal delivery there is a risk of injury to the mother due to the passage of the baby through the birth canal.
These injuries can involve tearing of tissue between the vagina and the anus which can be minor but if the trauma is extensive, sphincter muscles surrounding the anus can be partially or completely disrupted. These extensive tears are known as third and fourth-degree tears and despite surgical repair, some may result in life-changing problems for women. These life-long implications are both physical and psychological due to the potential issues of bowel incontinence, possible need for colostomy and intimacy difficulties such as sexual dysfunction within a relationship.
In response to rising anal sphincter injuries within our units, we formed a multi-disciplinary group of obstetricians and midwives to review our practice and seek a solution. After reviewing scientific literature, we arranged a visit to the unit in 2016 by Dr Jouko Pirhonen from Finland, who has pioneered an OASIS care bundle which consists of several measures aimed at reducing anal sphincter injuries. All maternity units within Northern Ireland were informed of Dr Pirhonen’s visit and were invited to his seminar in Altnagelvin Hospital in 2016.
His intervention has resulted in a reduction of anal sphincter injuries throughout Scandinavia, USA and Australia. Following a two- day workshop with Dr Pirhonen our OASIS team began planning the implementation of his OASIS care bundle which focuses on the following in prevention of tears:
- Clear communication between woman and midwife /obstetrician at delivery, no pushing at crowning
- Any position for first stage of labour
- Midwife/Obstetrician must have clear view of perineum in second stage of labour
- Perineal support
- If episiotomy required, correct technique at 60-degree angle is achievable with the use of Episcissors-60 (Episcissors-60 for medio-lateral episiotomies, NICE guidance MTG47, February, 2020)
- Risk assess for anal sphincter injuries (Be aware of risk but not an accurate prediction for third and fourth degree tears)
The OASIS care bundle has significantly reduced our 3rd and 4th degree tear rate over a 2-3 year period and supports the Royal College of Obstetricians and Gynaecologist (RCOG) Obstetric Anal Sphincter Injury care bundle.
Our project also relates to a joint statement from the Royal College of Midiwves (RCM) and RCOG who have encouraged all health professionals to adopt the care bundle into their practice to improve health outcomes for women.
Authors: Fiona Clarke, Brenda McClafferty and Mairead McCaffrey
NICE guidance MTG47 notes that Episcissors-60 show promise for use in the clinical area but there is currently not enough evidence to support a case of routine use throughout the NHS. The practice described in this example should be used for research purposes only, in line with the guidance recommendation for further research. The practice described in the example should not be used for wider routine implementation in the NHS at this time.
Example
Aims and objectives
Our aim with the implementation of the OASIS care bundle:
- Reduce third and fourth-degree tears within our maternity unit
- Aim for a fall in rates within a two-year period in line with the 2.9% national average
Our objectives included;
- Multi-disciplinary approach to training: Our project team leads recognised the importance of training all staff which included a multi-disciplinary approach involving midwives, obstetricians and students. Records of training and actions were important when interpreting dashboards and trends.
- Dashboards: Capture data on third and fourth degree tears rates with all vaginal births.
- Plan Do Study Act: Quality Improvement Methods applied to monitor and evaluate progress of OASIS care bundle.
- Purchase of Episcissors-60: Successful implementation of the OASIS care bundle also involved the purchase of Episcissors-60 as correct episiotomy technique at a 60-degree angle is achievable with these scissors and is significant component of the OASIS CARE bundle. A business plan was submitted to purchase epi-scissors 60 as a replacement for the traditional straight episiotomy scissors.
- Discussion Forms: Review all third and fourth degree tears/identify trends.
Our aim and objectives relate to recommendations published in the third and fourth-degree perineal trauma management, Green Top Guideline No.29, RCOG (2015) and NICE guidance Episcissors-60 for mediolateral episiotomy, MTG47, (February 2020).
Reasons for implementing your project
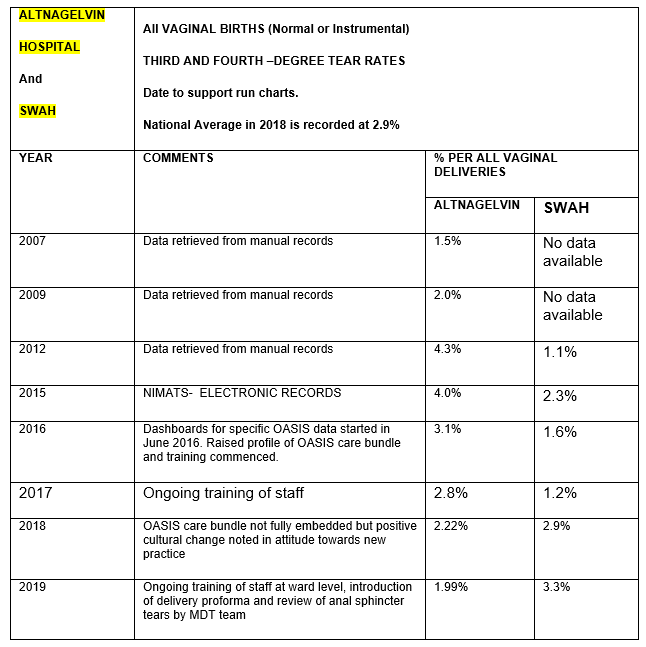
Our trust highlighted a significant rise in third and fourth-degree tears over a 6-year period from 2009-2015. Birth trauma to sphincter muscles surrounding the anus has life-long implications for women and their relationships. Changes in our practice methods at delivery required discussion and review in order to act for the well-being of women in our care. In addition to this, our project team leads also recognised the cost implications to the trust with our rising rates in anal sphincter tears over the past 6 years.
Prior to implementing any changes, a baseline audit was conducted of 20 vaginal births to observe current practice in perineal support. A wide variation in practice was noted in perineal support and maternal position for clear view of perineum. A pre–focus group was also conducted with our trust lead research nurse where staff could voice their views prior to implementing the OASIS care bundle.
Initial pre-focus sessions on raising awareness of this care bundle highlighted many midwives had concerns regarding maternal choice for labour and delivery. Midwives working in labour ward also had different levels of experience and confidence in performing an episiotomy with standard straight scissors.
At this time, episiotomies were cut with a straight scissor while ‘eyeballing’ the estimated angle of incision. Evidence has found that eyeballing the angel of 60 degrees is not accurate with many episiotomies carried out at 40-45 degrees. NICE 2020 support this by highlighting some studies have recorded only 22% of doctors achieving a 60-degree angle with straight scissors. No midwives achieved the recommended angle in these studies. The technique using the straight scissors may expose the women to an increase risk of an extended tear involving anal sphincter muscle if not performed at the recommended angle. In view of this, workshops were planned to not only provide training in OASIS methods at delivery such as communication on pushing, maternal position and perineal support but provided training on when to perform an episiotomy and how to use Episcissors-60. Episcissors-60 were purchased through an approved business plan.
To ensure compliance of use in the clinical area, quality improvement methods were applied and clinical champions identified to promote the change and support staff.
Financial implications of this rise in rates created further discussion when improving outcomes for not only women but the trust as a whole. Each injured woman requires a surgical procedure to carefully repair the sphincter muscle and is then followed up in a dedicated consultant led clinic 6 weeks later. One year after childbirth, women can still report ongoing symptoms of anal incontinence and urgent defecation related to their injury. Should the woman be experiencing any symptoms, trans-anal ultrasound and a colo-rectal surgical referral is required. The direct medical cost of treating each initial repair according to NICE is approximately £1289 per-person, excluding the cost of follow up and imaging. The NHS litigation authority published a review in 2012 and identified anal sphincter injuries as the fourth largest cause of litigation in obstetrics.
In the initial stages of our project, we identified 35 cases of anal sphincter injuries in a four -month period, therefore at that time 105 anal sphincter injuries could potentially be recorded for that year. The direct cost of repairing these injuries comes to 105 x £1289 = £135,345. This figure does not include additional costs of further reviews, imaging and surgery for women who are symptomatic after 12 months of initial repair. It also does not include any medio-legal claims as a result of anal sphincter injuries.
Purchase of epi-scissors 60 as an additional cost was considered when implementing the OASIS care bundle. However, as an essential component of the care bundle a business plan was therefore submitted. 30 Episcissors-60 were purchased as a replacement for the straight episiotomy scissors. Each pair of scissors had a purchase cost of £360 plus an additional cost of £63 for the sterilisation basket. Total capital investment was £12,690. The instruments were not likely to need replacement for many years of normal use and the sterilisation of the instrument cost £3.15 per scissor. Based on episiotomy rates in 2015, the overall annual cost for sterilisation for Episcissors-60 is £2,072. When indicated, correct episiotomy technique may reduce the risk of third- and fourth-degree tears. Purchase of the epi-scissors 60 requires a reduction of injured women by only 10 cases a year to make the purchase of this device cost-neutral.
In 2015, Altnagelvin Hospital had 81 repairs in theatre for anal sphincter injuries which resulted in a total annual cost of approximately £100,000. In 2018, 32 tears were recorded per annum which resulted in a significant reduction in initial theatre repair costs, approximately £40,000.
Implementation of ALL components of the OASIS care bundle has resulted in a decline in our third and fourth degree rates and a significant reduction in financial costs.
Demographics: Altnagelvin Hospital (2015) 2043 vaginal births. SWAH (2015) 893 vaginal births. Both hospitals are part of the WHSCT but are approximately 52 miles apart.
How did you implement the project
Implementation began with raising awareness with staff and patients following our two day workshop with Dr Pirhonen in March 2016. A multi-disciplinary team were identified to lead with this project which included Consultant Obstetricians, Lead midwives, labour ward manager, practice development midwife, risk management midwife, clinical champions (midwives), quality improvement department, lead research nurse.
Staff and patient information was provided through booklets, patient leaflets and posters.
A business plan was submitted to ensure introduction of Episcissors-60 which is a necessary component of the OASIS care bundle. The cost of their purchase has been outlined previously. Approval of this business plan proved challenging due to overall financial pressures within our trust In view of this, two pairs of Episcissors-60 were purchased per week through our labour ward budget. No additional funding was provided to this project. Valuable ‘time’ set aside by our OASIS team to ensure the implementation of this care bundle was the main ‘cost’ of our project.
Pre and post focus group sessions were held with staff to gain their views before and after the change and this was led by the trust research nurse. Responses were shared anonymously and provided the OASIS team with concerns and queries staff had in the clinical area regarding this care bundle. Subsequent training sessions addressed these issues to ensure engagement from staff in the clinical area.
Multi-disciplinary training on the OASIS care bundle began trust wide in 2016 and involved monthly workshops. Challenges faced were largely due to rotational staff within the maternity unit. Trained staff in OASIS methods is essential in labour ward. Clinical champions with a specific interest in this project were identified to help promote the change in the clinical area. Staff rotation due to service needs can result in slipping back to old practice methods. Constant review and display of dashboards on staff notice boards keep staff up to date and motivate staff to take ownership of practice within the labour ward.
To overcome the challenges of staff rotation, project leads ensured all new staff midwives and obstetricians received OASIS training as a priority when rotating to labour ward. All third and fourth-degree tears were reviewed by risk management and practice development midwife to identify any trends. Discussion forms were implemented for staff to complete in order to reflect on their delivery but this was not consistently completed by all staff. Some staff felt this created a ‘blame culture’ so trends were identified by practice development midwife reviewing patient health care records.
To ensure consistent staff engagement, progress was shared in the clinical area through newsletters, multi-disciplinary team meetings and visual dashboards in staff rooms.
Key findings
Altnagelvin
- When fully embedded, intervention with the OASIS care bundle has resulted in a significant reduction in tears.
- 81 tears were recorded in 2015 which is an annual rate of 4% for anal sphincter injuries.
- 41 tears were recorded in 2017 following implementation of OASIS methods which is an annual rate of 2.8%. This was less than the national average of 2.9% and was the first time our unit had been below the national average in 7 years.
- 32 tears were recorded in 2018 which is an annual rate of 2.5%.
- 32 tears were recorded in 2019 which is a rate of 1.99% which highlights a 50% reduction in anal sphincter injuries since 2015.
South West Acute Hospital (SWAH)
- When training in OASIS methods began in SWAH, anal sphincter injuries were already recorded below the national average at an annual rate of 2.3%.
- Following training, a further decline was recorded and rates in 2017 were confirmed at 1.2%.
- Unfortunately due to a loss of project leads/clinical champions and rotation of new obstetric/ midwifery staff, a rise in rates was noted. This resulted in a rise in the annual rate of anal sphincter injuries above the 2.9% national average in 2018-2019.
- In response to this new team leads were identified to refocus training and to address any regress towards old practice methods.
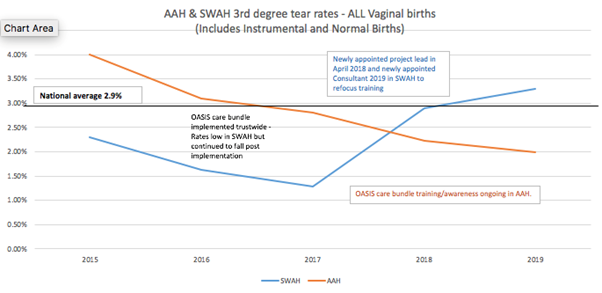
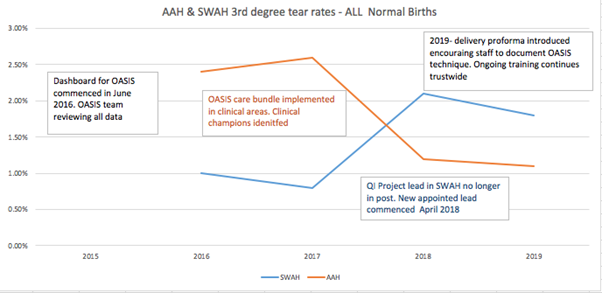
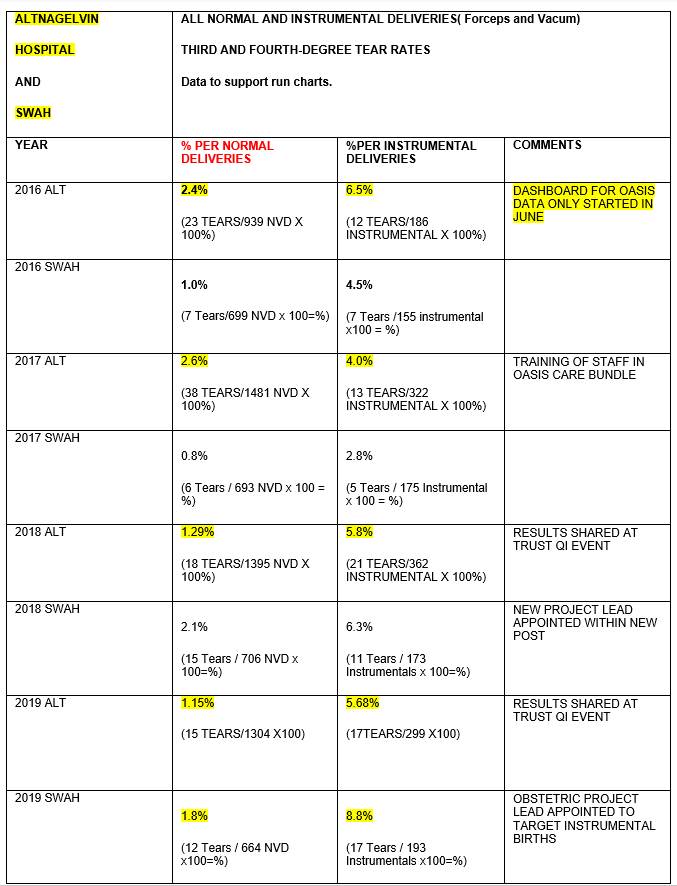
Findings indicate a steady decline in third and fourth-degree rates in normal vaginal deliveries since the implementation of all components of the OASIS care bundle. Despite a rise in the SWAH due to redeployment of project leads/rotation of staff as a contributing factor, both units are well below the national average of 2.9% since the implementation of the OASIS care bundle.
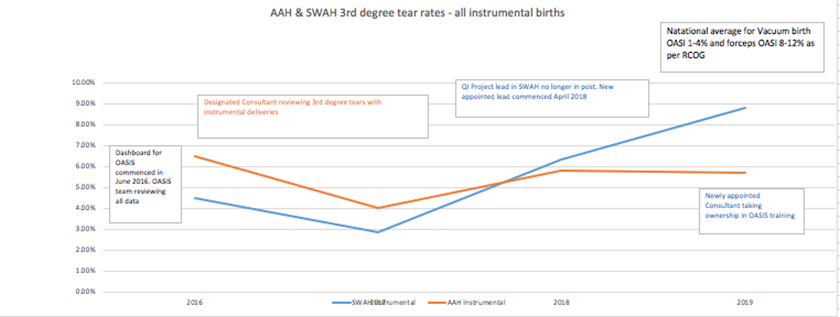
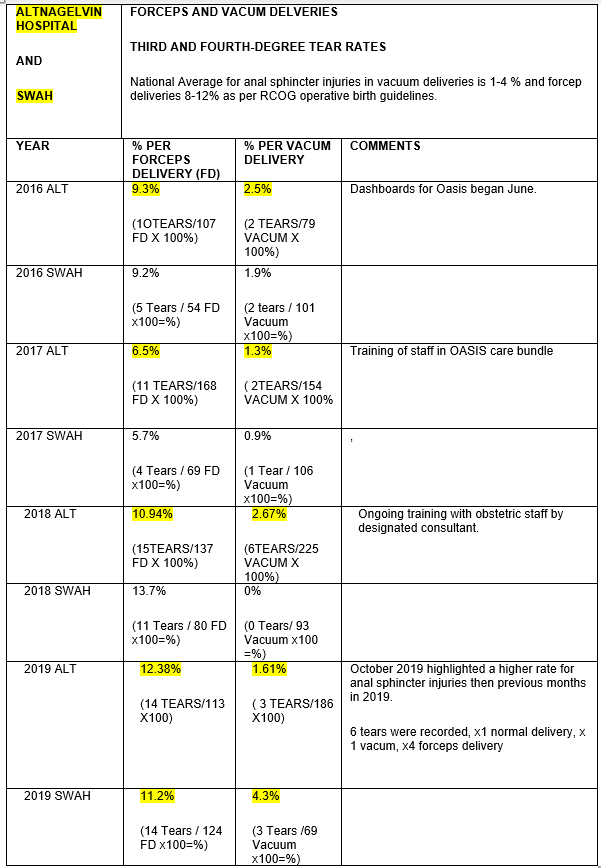
Findings support an initial decline in third and fourth-degree tears in instrumental deliveries across both sites since implementation of the OASIS care bundle in 2016. Subsequent rises in rates are due to a number of factors: rotation of obstetric trainees 6-12 months, obstetrician’s preference over forceps or vacuum, redeployment of clinical champions and project leads. The South West Acute Hospital did experience a significant change in staff during implementation of the OASIS care bundle which did have an impact on training. However, Altnagelvin Hospital maintained consistency with project leads and training which had a direct impact on anal sphincter injuries at instrumental deliveries.
Key learning points
When fully embedded the OASIS care bundle has reduced third and fourth-degree tears in our unit. Project leads and clinical champions are essential to promote and maintain new practice in the clinical area. Any disruption to training through redeployment of clinical champions and project leads can have a direct impact on change. New practices can slip and old practice methods can re-appear which contributes to a rise in rates as indicated on the graphs for one of our units.
A baseline audit of perineal support and communication at delivery is essential before introducing a change in any unit as it highlights variations in practice methods.
A change in staff attitudes and practice takes time. Pre and post implementation focus group sessions with staff are useful as it allows staff to feel involved with the change in practice and share their own experiences. Our team learned through these sessions that staff were initially fearful of a blame culture when reviewing practice at all deliveries. Some staff also questioned elements of the care bundle and were concerned regarding mother’s choice of position for labour and delivery. Many midwives did welcome more training on episiotomies. A year following implementation, a noticeable change in staff was noted and verbalised at a post implementation focus group session. Midwives felt more confident in performing episiotomies with Episcissors-60, had developed their knowledge, skills and understanding of third and fourth-degree tear prevention, did not feel women in their care had lost choice regarding their deliveries and over all felt positive about the OASIS care bundle methods.
Reviews of all third and fourth-degree tears by the project team identify trends and training needs. Common trends in the occurrence of anal sphincter injuries are primigravidas, induction of labour, and precipitate deliveries. Vacuum deliveries have a lower rate of OASIS than forcep deliveries. Delivery proformas capturing OASIS methods applied at delivery is a useful tool as documentation. It provided a clearer picture of the delivery during case management reviews.
A review of anal sphincter injuries at forceps or vacuum deliveries confirmed a higher incidence of rates with forceps and is highlighted in the table below. Further training for obstetric trainees on choice of instrument at delivery and its impact on anal sphincter injuries has been highlighted as key learning.
Additional learning and recommendations;
- Review and interpret episiotomy rates
- Check whether there has there been a reduction in first and second degree tears
- Check whether there has there been an increase in labial lacerations with OASIS methods
- Audit pain and perineal infection rates following use of Episcissors-60.
- Episcissors-60 show promise for use in the clinical area but further evidence is required to support a case of routine use throughout the NHS as set out in NICE guidance MTG47 (NICE, 2020)
- Clinical champions are essential when implementing a care bundle into the clinical area.