‘Artificial pancreas’ transforming the lives of thousands of children and young people with type 1 diabetes
The innovative hybrid closed loop (HCL) systems offer improved blood sugar control and can transform daily life for families managing this complex condition.

The NICE recommendation in December 2023 triggered a jump in uptake of hybrid closed loop (HCL) systems from just over one-third to nearly two-thirds in one year, and have reached about 3 in 5 eligible children and young people. Data from the National Paediatric Diabetes Audit (NPDA) shows that 62% were using HCL systems from April 2024 to March 2025, up from 36% in the same period the previous year.
Figure 1: Proportion of children and young people with Type 1 diabetes using a hybrid closed loop system from 1 Apr 2023 to 31 Mar 2025, in England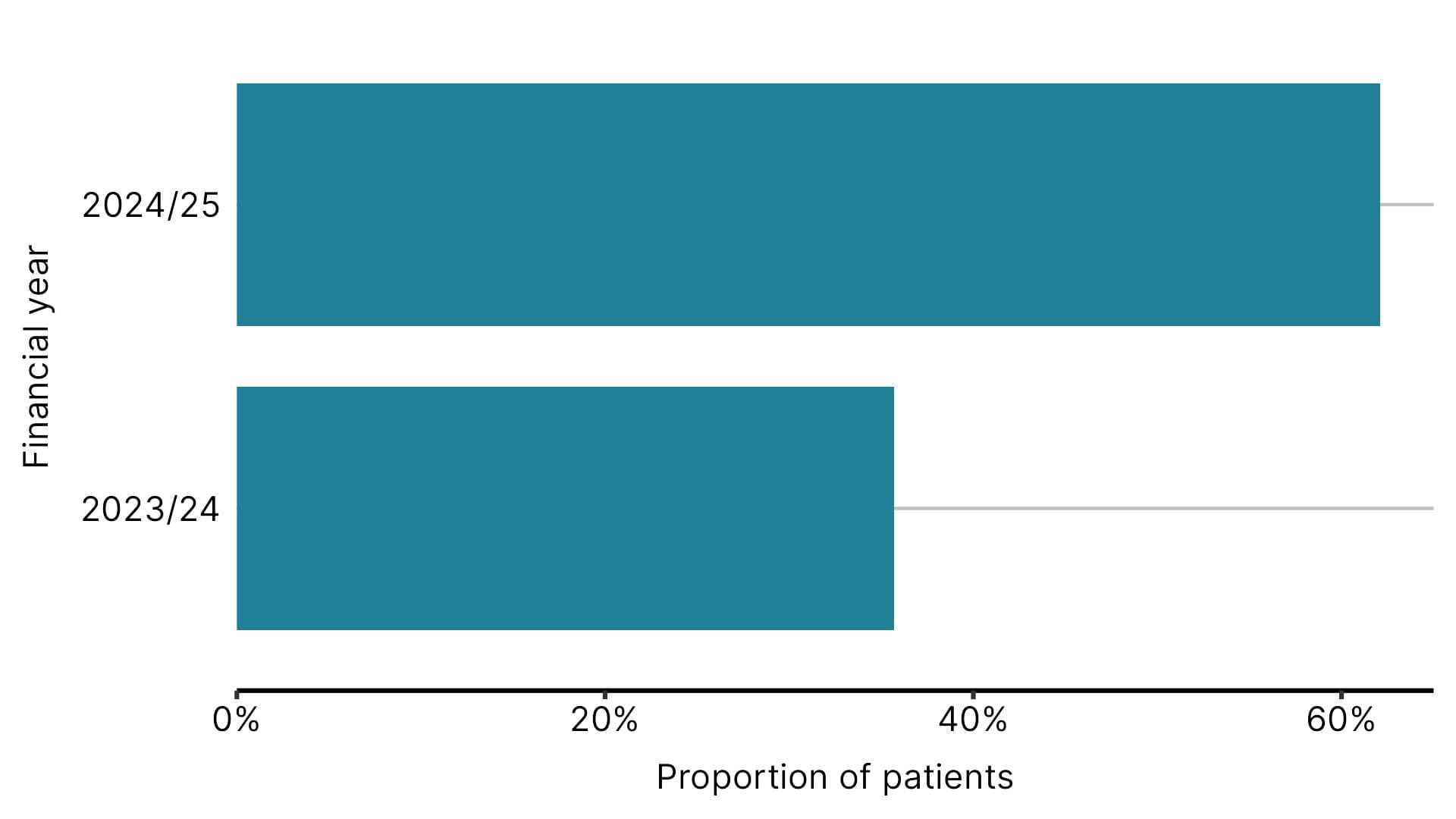
Claire Wragg’s son was diagnosed with type 1 diabetes in 2020, aged 12. “It was a shock. You go from a child that just eats and drinks what they want, when they want, to having to learn what carbs are, what foods they are in, how to control it."
Her son now uses a hybrid closed loop system. “It is hard to put into words how life changing this technology has been,” she said.
"I was naive to the impact of diabetes on the person and the family. You don't realise people are testing and injecting for every single meal - it encompasses your whole life."
In type 1 diabetes, the pancreas cannot produce insulin, causing high blood sugar levels. Without supplemental insulin, people with the condition would die. But too much insulin causes hypoglycaemia or hypos, where glucose levels become too low, which can also be dangerous. The goal is to keep blood sugar within a healthy range.
More than 30,000 children and young people are living with type 1 diabetes in England. Usual management involves finger prick testing and injecting insulin multiple times a day. HCL systems remove the need for this and help prevent blood sugar emergencies, which can be life-threatening.
Following NICE's landmark recommendation in December 2023, the majority of eligible children and young people with type 1 diabetes in England now benefit from this life-changing technology, demonstrating the real-world impact of NICE guidance on improving healthcare outcomes and quality of life. This remarkable progress shows the power of healthtech, when implementation is funded, to transform lives as much as any medicine.
Our independent assessment committee carefully evaluated not just clinical effectiveness but also quality of life impacts, which are proving to be transformative for thousands of children and their families.
Hybrid closed-loop technology is making a significant, life-changing difference for thousands of young people living with type 1 diabetes – improving their overall health, wellbeing and quality of life, and it’s encouraging to see this increase in take-up.
We’re proud to have contributed to the development of this transformative technology and continue to support efforts to ensure that everyone who is eligible can access it, regardless of their background or where they live.
What is a hybrid closed loop system?
A hybrid closed loop system, also referred to as an ‘artificial pancreas’, has three parts: an insulin pump, a continuous glucose monitor (a sensor that measures glucose levels at any given moment) and an algorithm that makes them ‘talk to each other’ and adjust insulin delivery. They are managed through a smartphone app.
The system automates most of the tasks, but it still needs some input before meals. Ms Wragg said: "Managing his diabetes is smooth now. You just pick up a phone, tell the app the carbs you are eating, and it injects the right amount of insulin. It doesn't do everything – his blood sugar levels still sometimes go high or low – but it takes so much hard work out of the process."
NICE agreed a 5-year roll-out plan with NHS England which will prioritise access to the technology for all children and young people, people who are pregnant or planning a pregnancy, and adults who are already using an insulin pump but it is not enough to control their blood sugar levels.
The NHS’s rollout of this innovative tech at pace and scale to thousands of children living with Type 1 diabetes is proving to be one of the biggest leaps in medical care for years following the publication of NHS England’s 5 Year Hybrid closed Loop Strategy, with highest ever investment.
I am particularly pleased to see that this transformative technology is enabling people- of all ages -with Type 1 diabetes to enhance their quality of life as well as delivering better clinical outcomes.
Game changer
South Yorkshire ICB has one of the highest uptakes of HCL systems in children and young people with type 1 diabetes: 652 were using a HCL system from April 2024 to March 2025. This is 77% of eligible children in the area.
Dr Allison Low, consultant paediatrician and clinical lead for diabetes in children and young people in South Yorkshire ICS, said the technology has had a very positive impact on children and their families:
“Kids describe it as a game changer. Many who were initially hesitant often say, ‘I don't know why I waited so long. It has changed my life.’ 99% of patients enjoy it and continue using it.
“We worked really hard in South Yorkshire to be early adopters of HCL systems, but we are also really positive about the NICE guidelines, which provide a safeguard to ensure continuing access for our patients.”
Uptake disparities
At a national level, there are regional variations in the uptake of the technology. There are also disparities by age, ethnicity and deprivation.
Figure 2: Proportion of children and young people with Type 1 diabetes using a hybrid closed loop system by age, deprivation and ethnicity
From 1 Apr 2024 to 31 Mar 2025, in England
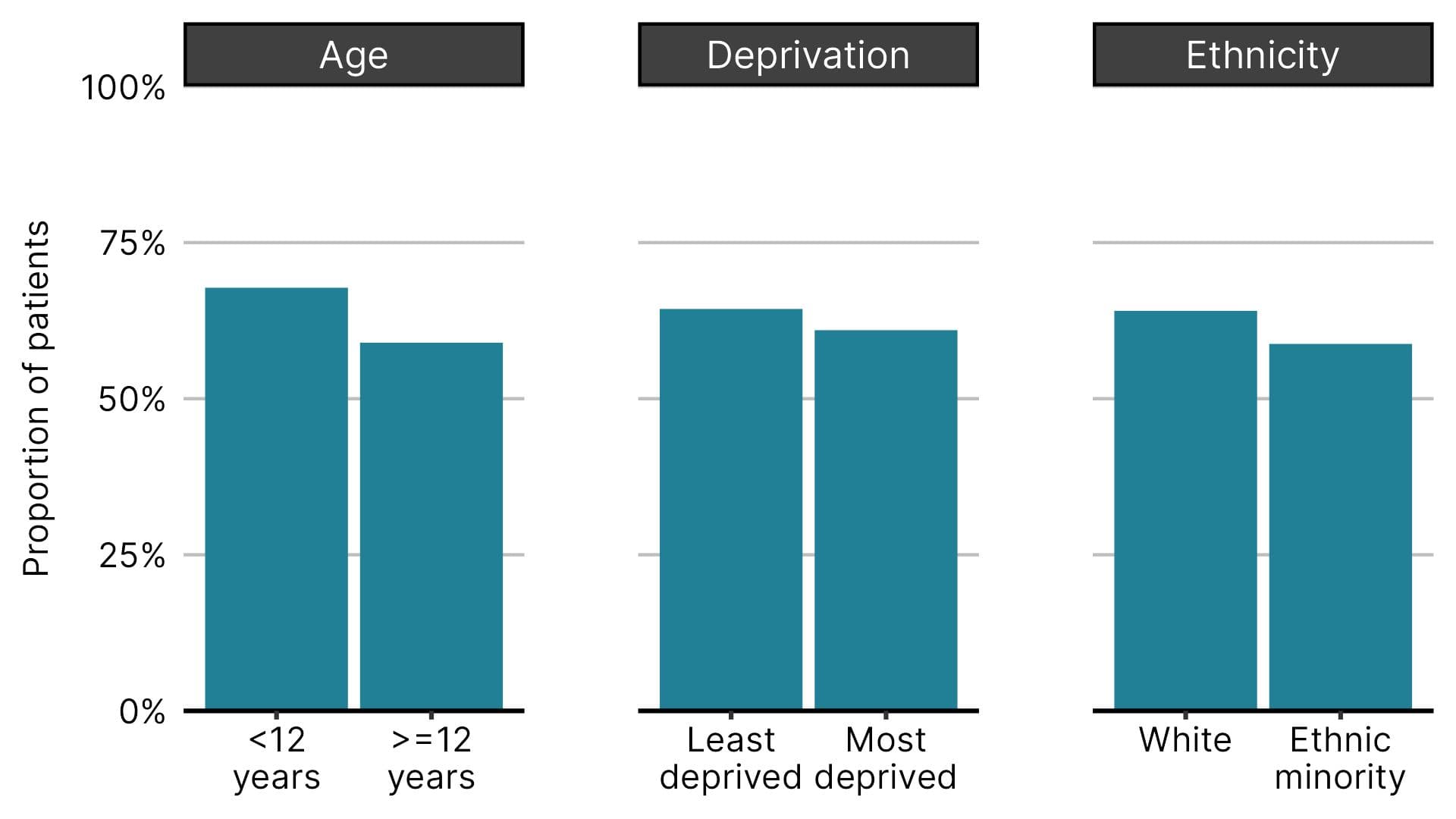
Uptake is highest among younger children, with 68% of under-12s using the systems compared to 59% of those aged 12 and older. There are also smaller differences in usage by ethnicity and deprivation.
Dr Brian Shine, chair of the diagnostics advisory committee that evaluated the technology said: “We pointed out that certain groups have poorer access to technology and medical care. People from socially deprived areas, some ethnic minorities, or those who don’t own smartphones - which are essential for using HCL systems - are at a disadvantage.”
NHS England has provided funding to pilot initiatives to reduce these gaps. Two trusts in South Yorkshire ICB used the money to hire a family support worker who focused specifically on children from ethnic minorities or more deprived backgrounds who were not using diabetes technology.
Health benefits
HCL systems have added benefits for children because they are sometimes less able to recognise the symptoms of high or low blood sugar. They also have less predictable exercise and eating patterns.
The systems deliver more precise insulin doses frequently, providing better long-term control and lowering the risk of diabetes-related complications.
Data for 2023/24 shows that HCL systems work best to control blood sugar levels compared with other technologies. Children and young people using HCL systems had the lowest HbA1c. This is the average blood glucose level over the previous 2-3 months.
Figure 3: Average HbA1c for children and young people with Type 1 diabetes using different diabetes-related technologies
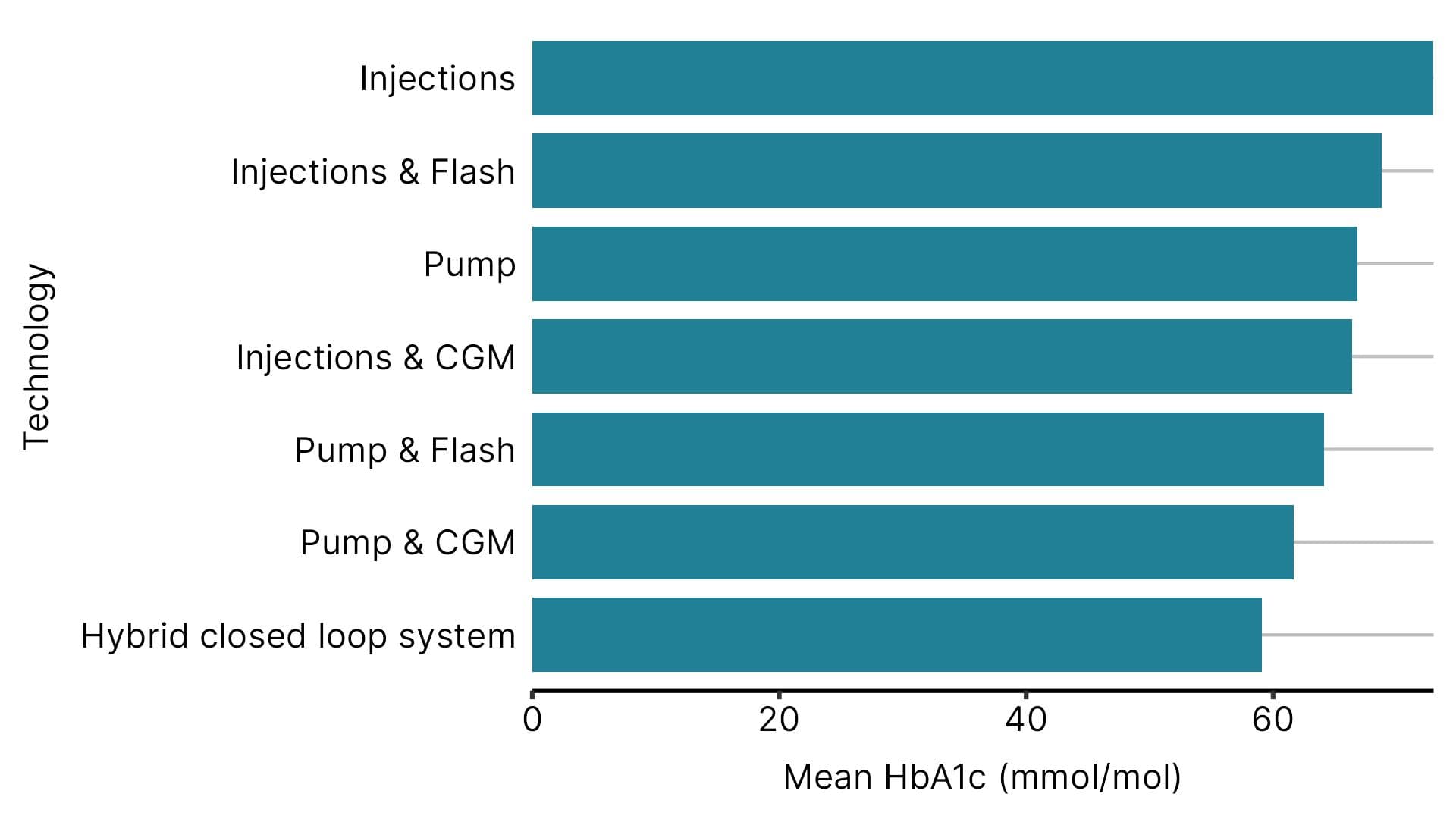
“His HbA1c while on this system have been amazing,” Ms Wragg said.
The pump should stop giving insulin if blood sugar levels become too low, which could result in fewer hospital admissions due to severe hypoglycaemia.
“It doesn’t stop all the hypos, but you can see where he is heading and step up at the touch of a button,” Ms Wragg added.
Blood sugar levels that are difficult to control can cause long-term complications such as blindness, kidney and heart disease, or stroke. While these health problems typically emerge in adulthood, early intervention can help avoid complications later in life.
Better quality of life
Dr Shine said: “Parents welcomed the recommendations. It relieves them of the mental burden of constantly monitoring their children.”
HCL systems promote independence and freedom: children don’t have to inject themselves and parents feel more confident with their children going out on their own.
“People talk about trusting the pump enough to let their child go on a sleepover for the first time or return to gymnastics class - childhood things. Parents have faith that the system will be increasing the insulin or giving an automatic correction if needed,” said Dr Low.
Improved sleep for both children and parents is one of the main benefits of HCL systems, as they don’t have to wake multiple times a night to check and treat glucose levels.
“It made a massive impact on his levels of stress and quality of sleep for both us as parents and him. You really do rely on it. Once you have it, going back to the basics is just an awful thought.” said Ms Wragg.
These benefits could also have a knock-on effect on employment and education. Ms Wragg added: “He’s now in college, and because his blood sugar levels are more controlled, he's able to concentrate and do better. He’s not having to have exams stopped while these levels come back into range, and obviously that will have a long-term effect on employment.”
What’s next?
HCL systems work much better than a human, but experts look forward to more advances:
“The technology is still improving; we anticipate that it will become more accurate and responsive. People would also love it if pumps got smaller, stickier, and didn't have to be changed as often.” said Dr Low.
Notes:
The figures for 2024/25 are provisional, and they may change once final data is published in March 2026. The data source is the National Paediatric Diabetes Audit (NPDA), published by the Royal College of Paediatrics and Child Health. The data includes children and young people with type 1 diabetes receiving care from a paediatric diabetes unit in England.