Overview
This guideline covers care and treatment for people with, or at risk of, chronic kidney disease (CKD). It aims to prevent or delay the progression, and reduce the risk of complications and cardiovascular disease. It also covers managing anaemia and hyperphosphataemia associated with CKD.
Last reviewed: 19 August 2025
We added links to relevant technology appraisal guidance in the sections on pharmacotherapy and managing anaemia. This is to provide easy access to relevant guidance at the right point in the guideline only and is not a change in practice.
This guideline updates and replaces NICE guidelines CG182 (published July 2014), NG8 (published June 2015), CG157 (published March 2013) and NICE evidence summary ESNM51.
Future updates:
August 2021: We have checked this guideline and plan to update the recommendation on oral antiplatelet therapy for reducing cardiovascular disease in people with chronic kidney disease. For more information, see the surveillance decision.
September 2021: We also checked this guideline to assess if chronic kidney disease should be highlighted as an HIV indicator condition. We did not have clinical consensus, so will not amend this area but will note the issue for consideration in the future. For more information, see the surveillance decision.
Recommendations
This guideline was updated in August 2021. There are new and updated recommendations on:
- investigations for CKD
- classification of CKD
- frequency of monitoring
- risk assessment, referral criteria and shared care
- blood pressure control
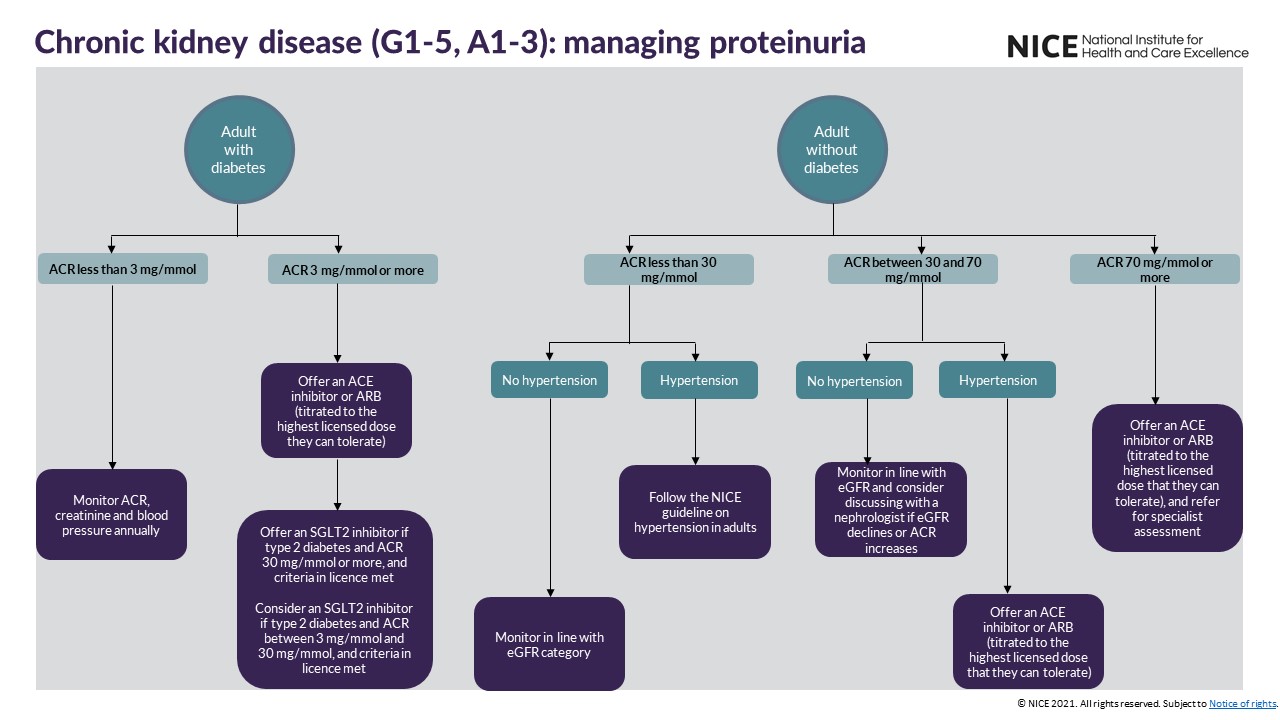
- medicines for CKD
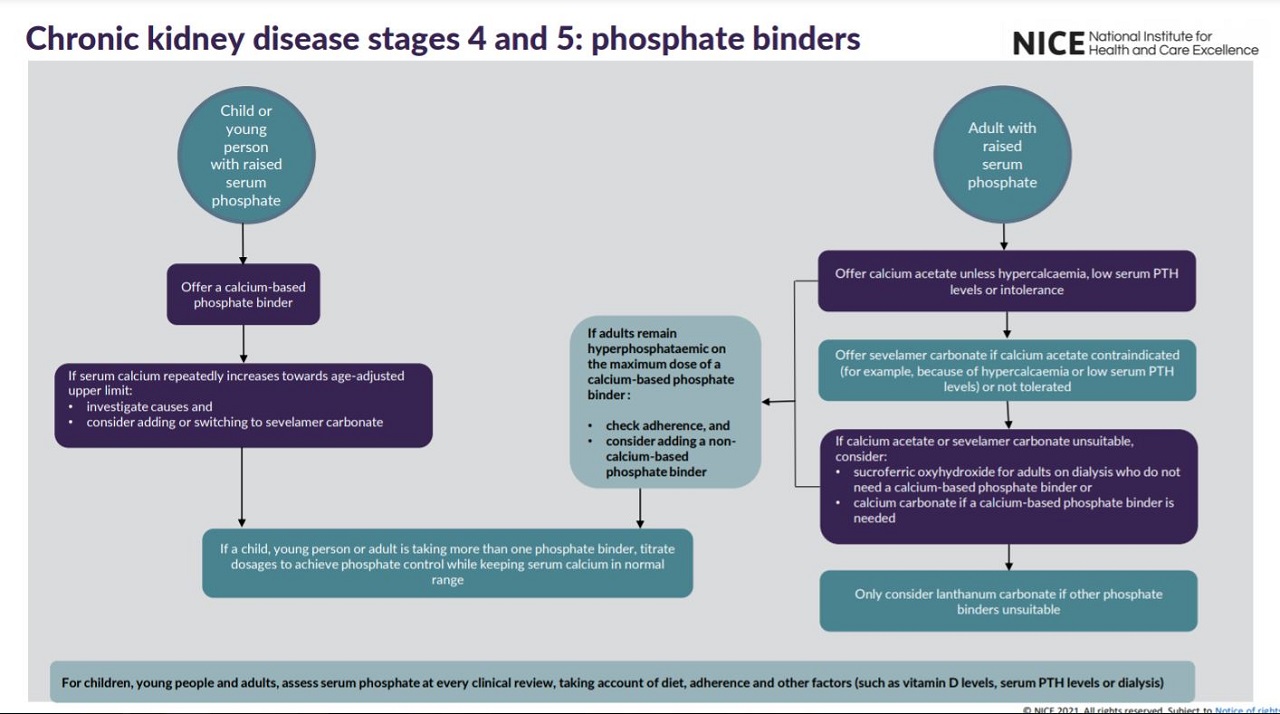
- phosphate binders to manage mineral and bone disorders
- glomerular filtration rate for diagnosing anaemia associated with CKD
- intravenous iron for treating anaemia associated with CKD
These supplement the existing recommendations on:
- information and education for people with CKD
- diagnosing and assessing anaemia associated with CKD
- managing anaemia associated with CKD
- assessing and optimising erythropoiesis in people with anaemia
- monitoring anaemia treatment
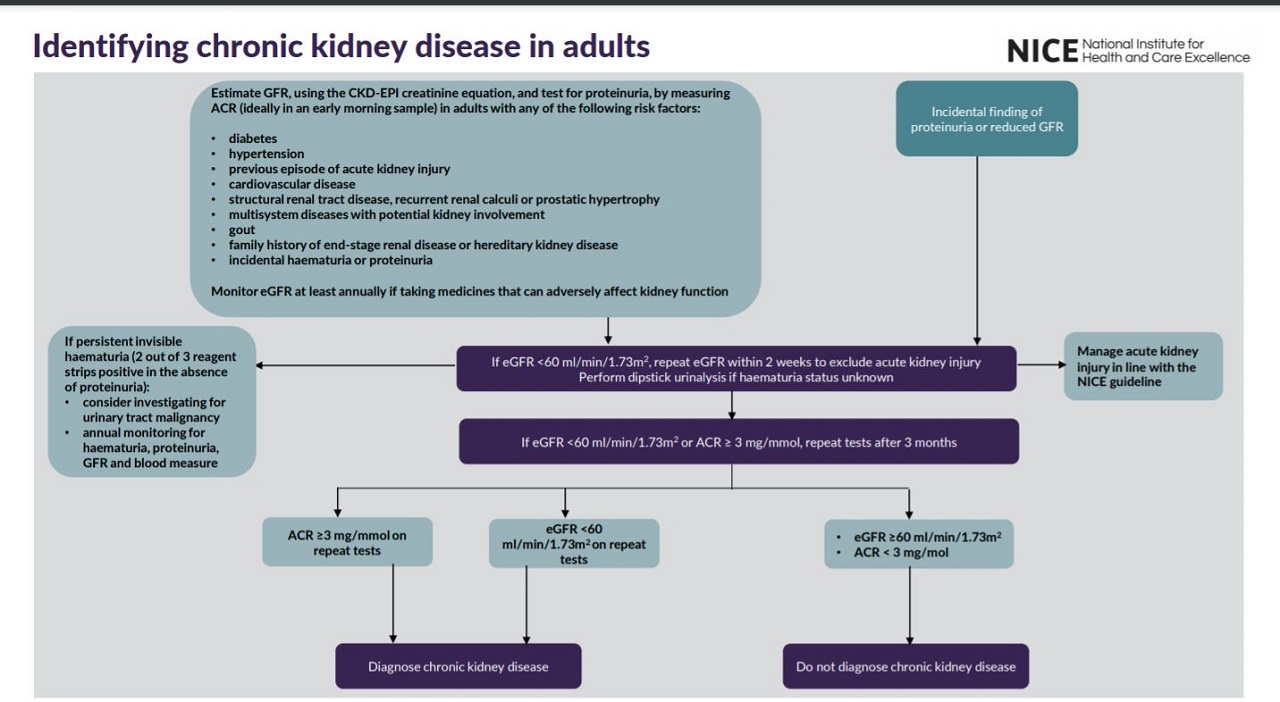
See visual summaries on the recommendations for identifying CKD in adults, phosphate binders and managing proteinuria.
Who is it for?
- Healthcare professionals
- Commissioners and providers
- People with chronic kidney disease, their families and carers
Guideline development process
How we develop NICE guidelines
Your responsibility
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems (adverse events) related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme.
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible.