Overview
This guideline covers diagnosing and managing epilepsy in children, young people and adults in primary and secondary care, and referral to tertiary services. It aims to improve diagnosis and treatment for different seizure types and epilepsy syndromes, and reduce the risks for people with epilepsy.
MHRA advice on antiepileptic drugs in pregnancy: Recommendations on carbamazepine, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, phenobarbital, phenytoin, pregabalin and zonisamide have taken into account the MHRA updated safety advice on antiepileptic drugs in pregnancy.
MHRA advice on valproate: Recommendations on valproate have been updated following publication of the MHRA guidance on the use of valproate, valproate use in people younger than 55 years, valproate use in women and girls and valproate use in men. Valproate must not be started for the first time in people (male or female) younger than 55 years, unless 2 specialists independently consider and document that there is no other effective or tolerated treatment, or there are compelling reasons that the reproductive risks do not apply. Valproate must not be used in women and girls of childbearing potential (including young girls who are likely to need treatment into their childbearing years), unless other options are unsuitable and the Pregnancy Prevention Programme is in place. Boys and men should be advised to use effective contraception (condoms, plus contraception used by a female sexual partner) throughout the valproate treatment period and for 3 months after stopping valproate. Men taking valproate who are planning a family within the next year should discuss potential fertility risks and treatment options with a healthcare professional.
MHRA advice on topiramate: Recommendations on topiramate have taken into account the MHRA guidance on the use of topiramate. Topiramate should not be used in women of childbearing potential unless the conditions of the Pregnancy Prevention Programme are fulfilled.
Last reviewed: 25 November 2025
We added links to relevant technology appraisal guidance in the section on treating childhood-onset epilepsies. This is to provide easy access to relevant guidance at the right point in the guideline only and is not a change in practice.
This guideline updates and replaces NICE guideline CG137 (January 2012) and NICE evidence summaries ESNM7, ESNM17 and ESNM37.
Next review: In January 2025, sulthiame was licensed for use in the UK. We are reviewing recommendations 6.4.2 to 6.4.4 in section 6.4 on self-limited epilepsy with centrotemporal spikes. See the guideline in development page for progress on the update.
How we prioritise updating our guidance
Decisions about updating our guidance are made by NICE’s prioritisation board. For more information on the principles and process, see NICE-wide topic prioritisation: the manual.
For information about individual topics, including any decisions affecting this guideline, see the summary table of prioritisation board decisions.
Recommendations
This guideline includes recommendations on:
- referral, assessment and diagnosis
- information and support
- principles of treatment, treating epileptic seizures and treating childhood-onset epilepsies
- non-pharmacological treatments
- status epilepticus, repeat or cluster seizures, and prolonged seizures
- managing comorbidities
- reducing the risk of epilepsy-related death
- referral to tertiary services
- epilepsy specialist nurses and transition from children’s to adults’ services
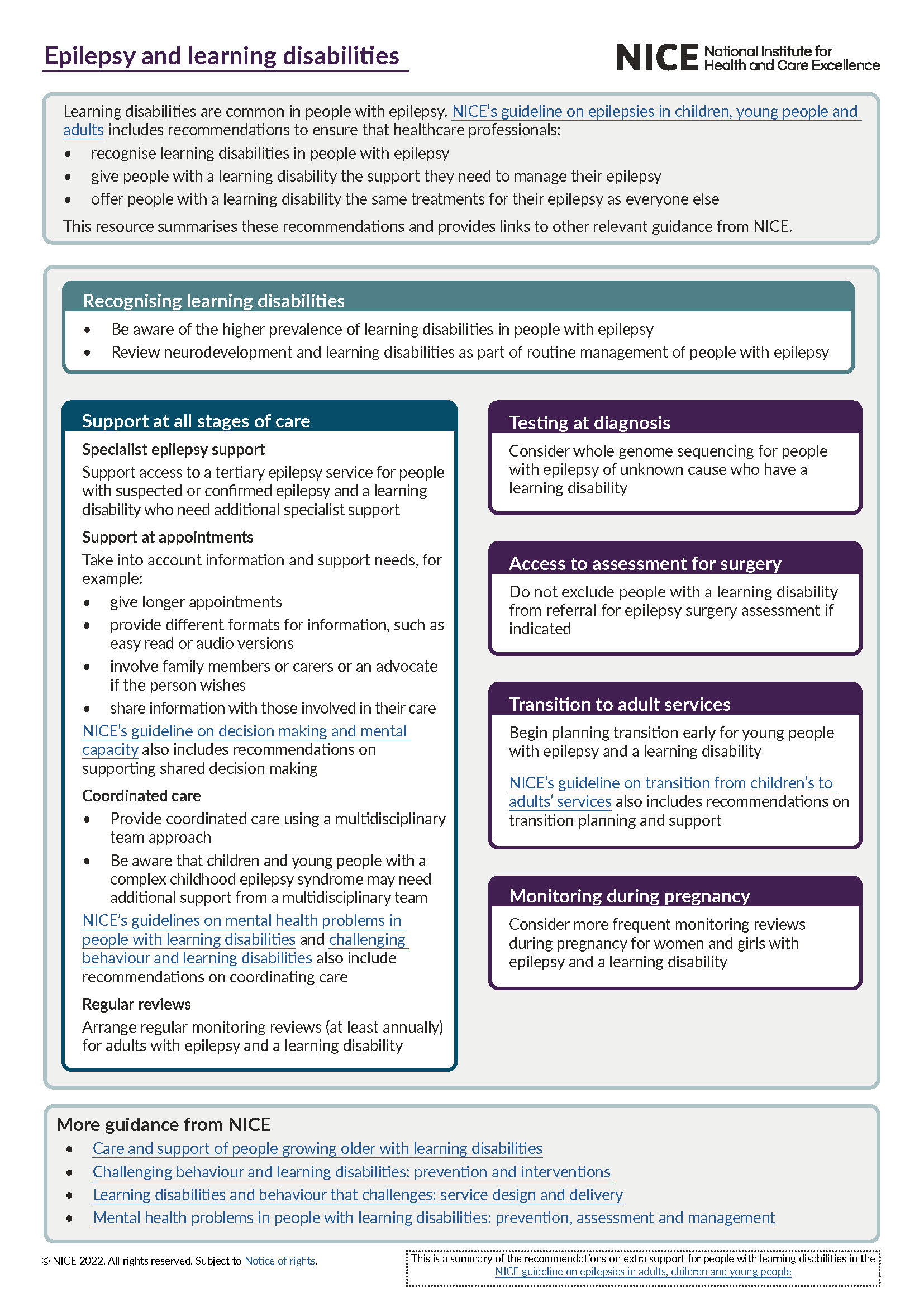
See the 1-page visual summary of the recommendations for people with epilepsy and a learning disability.
Who is it for?
- Healthcare professionals in primary, secondary and tertiary care
- Commissioners, providers and voluntary organisations
The guideline may also be useful for people with epilepsy, their families and carers to understand the care NICE recommends and support shared decision making.
Guideline development process
How we develop NICE guidelines
Your responsibility
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems (adverse events) related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme.
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible.