NICE has made six times more lung cancer treatment recommendations over the past ten years than in the previous decade
We have also recommended osimertinib for routine use on the NHS today.

The treatment landscape for lung cancer has changed considerably in the last decade, and survival rates have improved.
In the last 10 years NICE has made 48 positive recommendations for lung cancer treatments, 6 times more than in the previous decade.
Jules Fielder was diagnosed with stage 4 lung cancer in 2021, aged 37. She is not a smoker and did not have any of the symptoms commonly associated with lung cancer, such as breathlessness or a cough.
“Lung cancer has no labels; it can happen to anybody at any age.”
Ms Fielder has been on osimertinib since 2021. Despite having to reduce the dose initially due to side effects, she said it is “an amazing drug” that has allowed her “to live very well”.
“When I had my first scan after three months of being on osimertinib, the cancer had shrunk by 90% in my lungs. And I have stayed stable since that day.”
“And because they are tablets, we don't have to go to hospitals and be strapped to machines,” she added.
Around 95 people die of lung cancer every day in the UK. It is the most common cause of cancer death and kills more women than breast and ovarian cancer combined.
One of the myths about lung cancer is that only people who smoke get it, experts have said. “If you have lungs, you can get lung cancer. Around 15% of patients with lung cancer have never smoked,” said Dr Tom Newsom-Davis, consultant medical oncologist at Chelsea and Westminster Hospital, and Chair-Elect of the British Thoracic Oncology Group (BTOG).
Dr Jesme Fox, medical director of the Roy Castle Lung Cancer Foundation added: “Another misconception is that if you get lung cancer, there is no hope. That is not true at all.”
“If we pick up lung cancer early, then surgery and radiotherapy are potentially curative. And we have seen many advances in the last 10 to 15 years, there are a lot more treatment options now than there used to be.”
Transforming lung cancer treatment
Dr Lynn Campbell, consultant medical oncologist at Belfast City Hospital and committee member for the NICE lung cancer guidelines said: “When I started as a consultant back in 2010, for most stage 4 lung cancer patients the conversation would be around a 6-to-9-month survival. Whereas now with all the additional therapies available, we have stage 4 patients surviving 6-7 years.”
NICE has made 48 positive recommendations for lung cancer treatments since 2015. This includes innovative treatments such as targeted therapies—which are given as a tablet and work against specific mutations—and immunotherapy —which uses the body’s immune system to attack the cancer.
A recommendation is positive when a treatment is recommended, optimised or recommended for use within the Cancer Drugs Fund (CDF). Over the past ten years, 86% of our lung cancer recommendations have been positive.
Figure 1: Number of lung cancer treatment recommendations made by NICE, 2001-2024
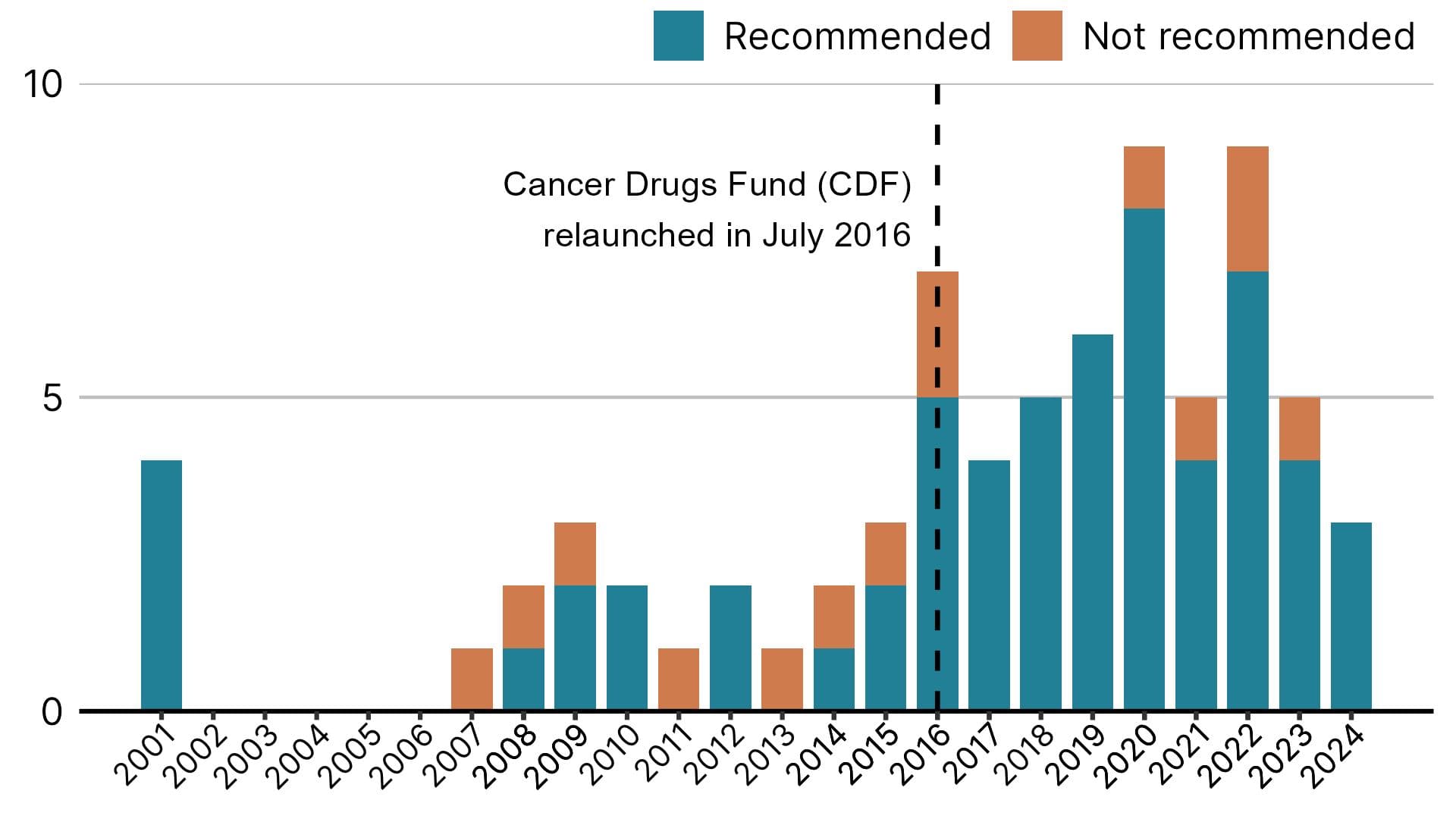
The number of lung cancer recommendations has increased since 2016, when the CDF was relaunched. NICE can recommend drugs for use in the CDF while more evidence is collected, which allows wider and faster access to cancer treatments.
Dr Newsom-Davis said: “At the moment I have every lung cancer drug that I need that is licensed. That reflects how the medical and clinical oncology community, respiratory physicians, and surgeons, have engaged with NICE and collaborated in getting medicines to NICE appraisals and providing support in that process.”
Dr Fox added: “It is crucial that we all keep up to date with what is available, and the NICE treatment pathway for non-small cell lung cancer has made a huge difference. It is a very easy way to keep track of recommended treatments.” NICE has published the treatment pathways as part of its lung cancer guidelines.
NICE has produced useful and usable lung cancer guidelines to help practitioners provide the best standards of care to patients.
We have recommended multiple lung cancer treatments that have contributed to better survival, but lung cancer remains the biggest killer among cancers in England.
We are committed to continue focusing on what matters most to support patients, practitioners, and the NHS.
Early diagnosis
The expansion of available treatments has led to better outcomes, but late diagnosis is still an issue. There are usually no symptoms in the early stages. Some symptoms can be mistaken for other conditions, which is a particular problem for people who have never smoked.
“I had back pain that was diagnosed as sciatica and my voice was a little husky. The pain in my arm had been diagnosed as tennis elbow. Those symptoms were missed,” said Ms Fielder.
It was not until she found a lump on the side of her neck that the cancer was discovered. It had already spread to her spine and pelvis.
“We need more awareness and a greater knowledge of symptoms. I have met ladies aged 19, 20, 22 who are sadly gone now because they did not have a chance to fight.”
The most important factor in survival is early diagnosis. Survival rates have improved over the last decades and are expected to continue doing so, but the UK has lower survival rates than comparable countries.
Figure 2: Lung cancer survival in England. 1 and 5 year index net survival for adults diagnosed from 2005 to 2020 and followed up to 2021

About 1 in 12 lung cancer patients (8.6%) diagnosed in 2005 survived their cancer for five years or more, which improved to about 1 in 5 patients (19.8%) by 2016. Less than 1 in 3 patients (28.9%) diagnosed in 2005 survived for at least one year. By 2020, this improved to about 1 in 2 patients (48.1%).
These figures are estimates for all lung cancer patients in England, but they do not reflect survival prospects for any individual patient. In addition to the stage of the cancer at the time of diagnosis and available treatments, survival depends on other factors such as genetic mutations and the general health and fitness of the individual.
NHS England’s lung health checks, which aim to catch the disease early, have been available in some parts of England since 2019. Following the success of the scheme, a national lung cancer screening programme was announced last year. People aged 55 to 74 at increased risk of lung cancer are invited for specialist scans.
What’s on the horizon?
“The lung cancer screening programme has been a huge success already across England. We hope to get better at that to identify more people at early stages,” said Dr Fox.
Clinical experts agree that we are moving into an era of more sophisticated treatments.
“We anticipate more targeted and immunotherapy drugs in the future. Trials for lung cancer vaccines are ongoing,” she added.
Dr Newsom-Davis said: “Novel therapies have been revolutionary so far, but they don’t work for everyone, they don’t work forever, we need them to work for more people and for longer.”
Notes:
Some treatments can be recommended more than once if the guidance is reviewed and modified.
The recommendation for osimertinib published today is for the adjuvant treatment of stage 1b to 3a non-small-cell lung cancer (NSCLC) after complete tumour resection. NICE also recommends osimertinib for other indications such as metastatic NSCLC.