Simple home test prevents thousands of unnecessary bowel cancer referrals
A simple home test is sparing thousands of people from unnecessary hospital investigations for bowel cancer, while helping them get faster answers about whether they have the disease – with new data showing the impact of NICE's recommendation to use the test.

In 2024/25 there were 140,000 fewer referrals for suspected bowel cancer than expected.
The faecal immunochemical test (FIT) detects small amounts of blood in poo, which can be a sign of bowel cancer. Bowel cancer is the second biggest cancer killer in the UK, affecting the large bowel including the colon and rectum. Most cases are diagnosed in people over 50, but it can affect anyone.
Since the test was rolled out, urgent referrals for suspected bowel cancer have declined. Yet the number of cancers detected has remained stable, meaning the test is successfully identifying patients who genuinely need urgent investigation and those who can be safely reassured they do not have cancer. NHS England data shared with NICE shows the test is making a real difference to patient experience and reducing pressure on NHS services.
NICE guidance drives adoption
NICE issued guidance in 2023 recommending FIT for assessing patients with symptoms of bowel cancer, building on earlier guidance that recommended GPs offer the test to some categories of people with relevant symptoms.
Since then, adoption has increased steadily. The proportion of urgent referrals accompanied by a FIT result has risen from under 60% in June 2023 to almost 80% in June 2025.
Dr Kashif Siddiqui, a GP at St Georges Medical Practice in Essex, said: "Almost all urgent referrals go with a FIT result now, unless there is strong evidence that someone needs to be referred right away.”
By doing this, patients can avoid unnecessary trips to hospital for more investigations, making the system work better for everyone.
Dr Baljit Singh, colorectal surgeon at University Hospitals Leicester NHS Trust and committee member for NICE's FIT guidance, said: "We have very high compliance – around 90% of primary care referrals in our area come with a FIT result. There are always people who can't do a FIT test, maybe because of frailty, learning difficulties, or other reasons."
Fewer unnecessary referrals, same cancer detection
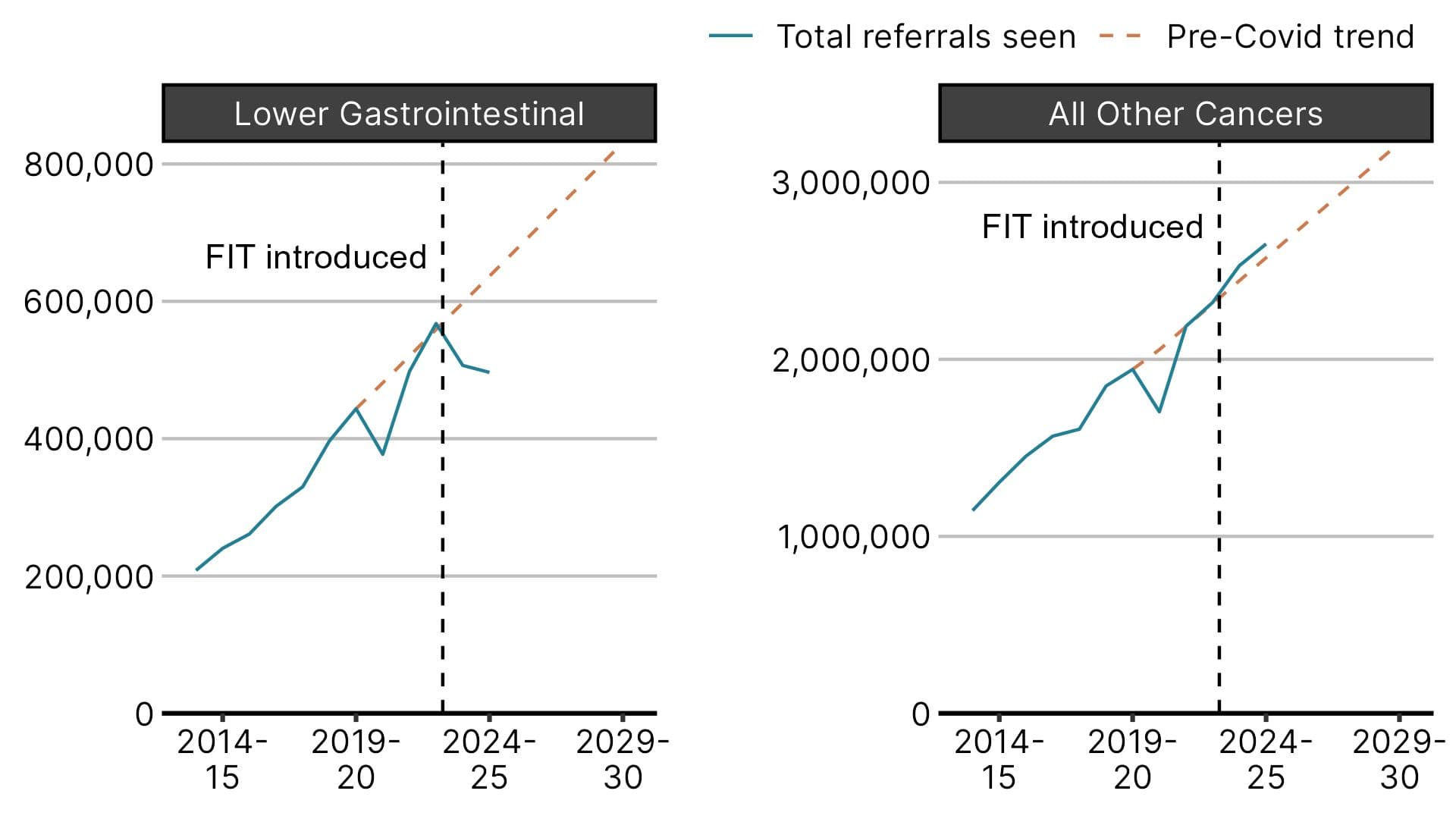
The introduction of FIT has helped GPs make more targeted referrals. Urgent primary care referrals for suspected bowel cancer have fallen over the past two financial years, even as referrals for all other cancers combined continue to rise.
NHS England data shows that in 2024/25 there were 140,000 fewer referrals than expected – 22% below the pre-pandemic trend. This suggests that FIT is helping to identify which patients need urgent investigation and which can be safely managed in primary care. Meanwhile, referrals for all other cancers have remained broadly in line with the pre-pandemic trend.
Figure 1: Urgent referrals for suspected cancer in England, by financial year
Dr Singh said: "In the past, people with symptoms went straight for investigation, but for many there was no link between their symptoms and cancer. Now, most people with symptoms do a FIT test first. Depending on the result, they will either have further investigations or be managed by their GP."
Research published last year analysed over 10,000 patient records from nine NHS Trusts in the South West to evaluate the impact of FIT. It showed that GPs widely adopted the test, leading to fewer colonoscopies and waiting times returning to pre-pandemic levels.
Faster answers for patients
People are also getting faster answers about whether they have bowel cancer. Faster diagnosis means patients can start treatment sooner if they have cancer, or be reassured more quickly if they don't.
The NHS lower gastrointestinal Faster Diagnosis Standard says patients urgently referred for suspected cancer should find out whether they have cancer within 28 days. As use of FIT has increased, performance against this standard has improved notably. The improvement is largely driven by people being ruled out for cancer, as this group is larger than those diagnosed with the disease.
Figure 2: Proportion of people meeting the 28-day Faster Diagnosis Standard in England, by month
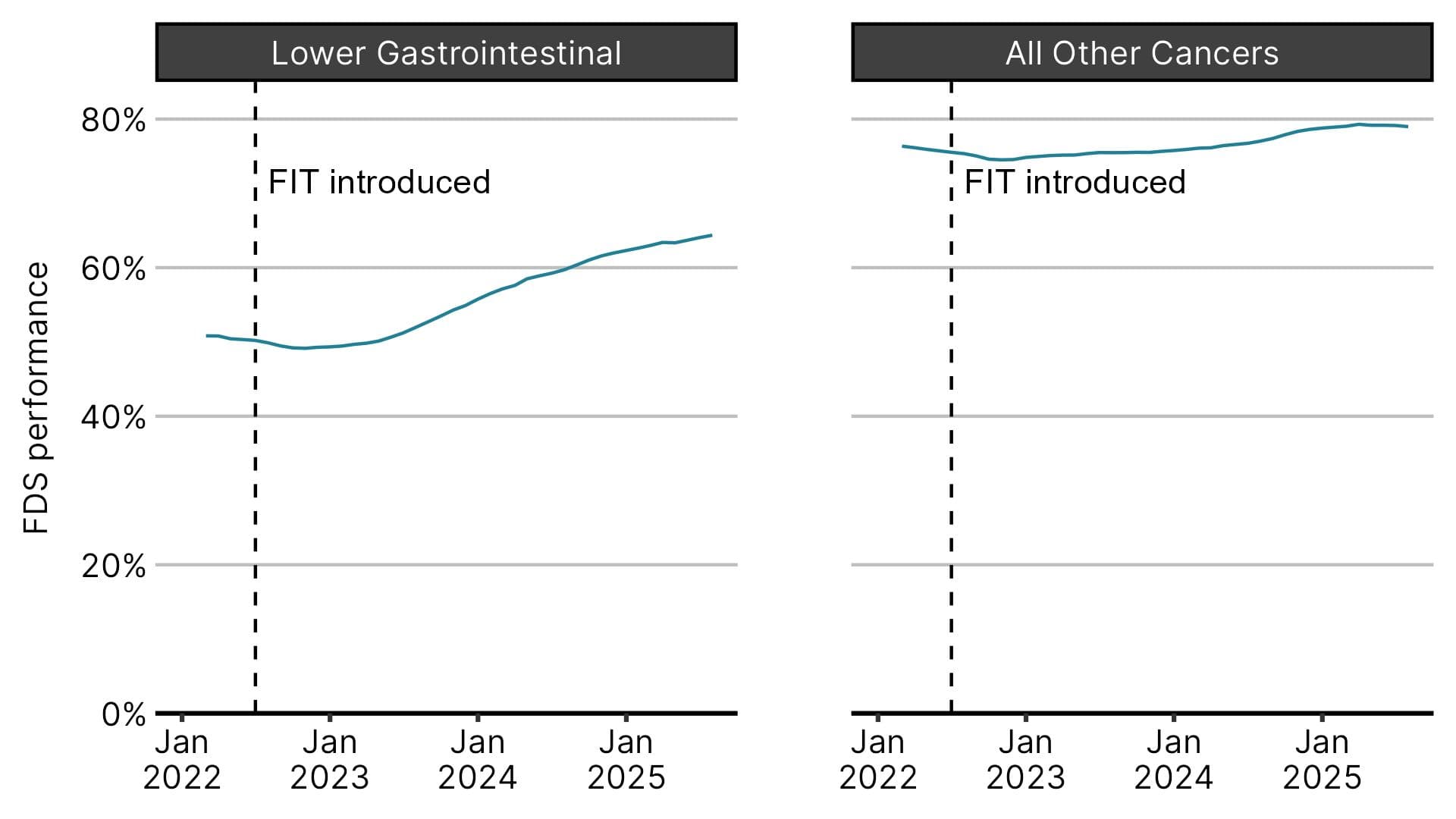
The lower gastrointestinal Faster Diagnosis Standard has improved by 14 percentage points since FIT was introduced, from 50% in July 2022 to 64% in August 2025. For all other cancers combined, the standard improved by just four percentage points in the same period. But despite this progress, the lower gastrointestinal FDS continues to lag behind other cancers.
It is encouraging to see the excellent adoption in primary care of this technology to avoid unnecessary procedures, reduce patient anxiety, and make more efficient use of NHS resources.
Eric continued: "By using FIT, clinicians can more safely and quickly reassure people who are unlikely to have cancer and remove them from the NHS waiting list for a cancer referral. This is not only better for the patient, but frees up appointments for people who do have cancer to be seen faster, and that will improve their chances of a positive outcome following treatment.
"NICE is committed to keep focusing on what matters most to support cancer pathways and deliver better outcomes for patients."
NICE's endorsement of the use of FIT in patients with suspected bowel cancer has been a major driver in its rapid implementation and uptake across the NHS, thereby allowing those patients at greatest risk access to urgent investigation when most needed.